Altered Blood Vessel Repair Process ID’d in GPA Remission Patients
Impairments of ECFCs could explain recurrent nature of AAV, researchers posit
The function of endothelial colony-forming cells (ECFCs) is impaired in people with granulomatosis with polyangiitis (GPA) — a type of ANCA-associated vasculitis (AAV) — who are in disease remission, according to a recent study.
Impairments in ECFCs’ ability to repair damaged blood vessels — their normal role — even in a state of remission could underlie the recurrent nature of AAV, the researchers suggested.
“These findings highlight the need for further studies concerning endothelial function in patients with GPA, which may lead to the development of new therapeutic approaches,” they wrote.
The study, “Impaired repair properties of endothelial colony-forming cells in patients with granulomatosis with polyangiitis,” was published in the Journal of Cellular and Molecular Medicine.
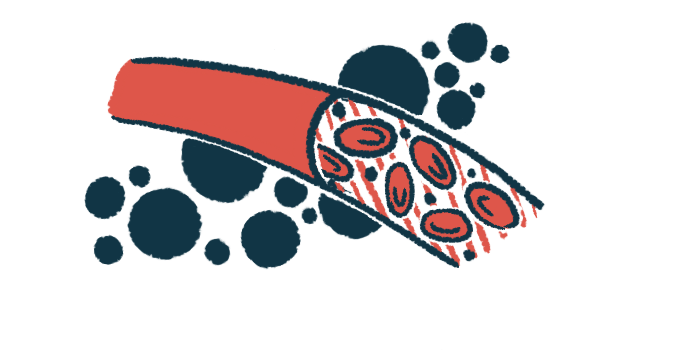
As with other AAV types, GPA is marked by inflammation and damage to small blood vessels as a result of self-reactive antibodies called ANCAs that bind to certain immune cells, called neutrophils and overly activate them. This leads to a loss of integrity of endothelial cells, which line blood vessel walls.
ECFCs are a type of self-renewing endothelial cell with properties that support forming new blood vessels from existing ones, a process called angiogenesis. This can help repair vascular damage, or damage affecting the blood vessels.
Their impairment leads to deficits in blood vessel repair that have been previously linked to vascular diseases, but the properties of ECFCs in patients with AAV have not been well explored.
Researchers isolated ECFCs from the blood of GPA patients at the State University of Campinas, Brazil and examined their properties in cell cultures. Cells from healthy volunteers were also collected and used as control samples.
Patients were either newly diagnosed and not yet treated or in remission and undergoing follow-up without immunosuppressive treatments for at least two years. All were positive for antibodies against proteinase 3 (PR3), the type of ANCA usually associated with GPA.
Samples from eight patients — five with disease activity and three in remission — as well as eight healthy controls were successfully cultured and analyzed.
The number of ECFC colonies that grew in cell cultures did not differ between controls, patients with active disease, and remission patients, although a single GPA patient with active disease had a colony count four times higher than that observed in the other samples.
ECFCs of patients and controls were similar in form and produced genes associated with endothelial cells. While angiogenesis was comparable in general between patients and controls, patients in remission, but not those with active disease, had a decreased capacity for blood vessel formation compared with healthy people, analysis showed.
A migration assay was done to investigate the response of the ECFCs to a stimulus to induce reparative processes. Essentially, each cell culture was gently scratched and monitored for how long it would take for the ECFCs to travel to the site of the scratch and repair it. No significant differences were observed between patient and control cells.
In one patient with active disease, cell cultures of ECFCs were obtained both before treatment and again after remission induction with cyclophosphamide. ECFCs collected after remission showed significantly lower migration capacity compared with cells collected before remission.
To account for the fact that factors present in plasma — the liquid component of blood — can also influence ECFC function, ECFCs were incubated overnight in plasma collected from either patients with active disease or healthy controls, and the migration assay was performed.
ECFCs from patients in remission showed significantly lower migration capacity compared with healthy cells, even after incubation in healthy plasma, again suggesting altered ECFC function among remission patients.
The findings “revealed the possibility of intrinsic endothelial cell changes in patients with GPA, compromising their angiogenic capacity,” the researchers wrote. “Future studies are needed to identify factors that may improve vascular homeostasis in patients with GPA.”