Discussion
Discussion
Tavneos (avacopan) for ANCA-associated vasculitis
Last updated Aug. 22, 2024, by Marta Figueiredo, MS

What is Tavneos for ANCA-associated vasculitis?
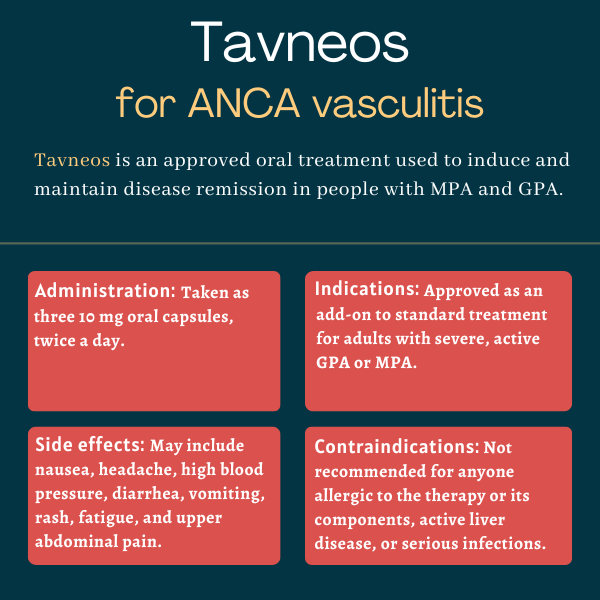
Tavneos (avacopan) is an oral therapy approved for adults with severe and active microscopic polyangiitis (MPA) and granulomatosis with polyangiitis (GPA), the two most common types of ANCA-associated vasculitis (AAV).
The treatment, to be used in combination with standard therapy, including glucocorticoids, is designed to induce and maintain disease remission in people with the autoimmune disorder. It works by modulating the body’s immune response.
Tavneos was originally developed by ChemoCentryx, which was acquired in October 2022 by Amgen, which holds the therapy’s rights in the U.S. Otsuka Canada Pharmaceutical has marketing rights to the therapy in Canada, while Kissei Pharmaceuticals hold those rights in Japan. CSL Vifor Pharma holds the therapy’s rights in nearly all other countries, including those in Europe.
Therapy snapshot
| Brand name: | Tavneos |
| Chemical name: | Avacopan |
| Usage: | Used to treat adults with MPA or GPA; can help induce and maintain disease remission |
| Administration: | Oral capsules |
How does Tavneos work?
ANCA-associated vasculitis is an autoimmune disease in which self-targeting antibodies, called ANCAs, result in the overactivation of neutrophils, a type of immune cell. This overactivation promotes inflammation and damage to small blood vessels.
Part of ANCAs’ damaging effects are driven by the neutrophil-induced activation of the complement system, a family of proteins that plays an important role in the immune response. This leads to the generation of C5a, a complement protein that binds to C5a receptors (C5aR) on immune cells and on cells that line blood vessels.
When bound to its receptor, C5a signals to immune cells to gather to the site, promoting the accumulation of immune cells and inflammatory signals near small blood vessels, damaging them.
Tavneos contains an orally available small molecule that selectively binds to C5aR, preventing its interaction with C5a. This reduces the number of immune cells that wrongly rush to these sites in the body. In this way, Tavneos works to reduce inflammation and damage to small blood vessels in AAV.
Who can take Tavneos?
Tavneos was approved by the U.S. Food and Drug Administration in October 2021 as an add-on to standard treatment, including glucocorticoids, for adults with severe and active GPA and MPA. The decision made Tavneos the first approved treatment for AAV in the U.S. in more than a decade, and the first oral C5aR suppressor to be approved for the autoimmune disease.
The therapy also is approved for the same indication in the European Union, as well as in Australia, Canada, Japan, Switzerland, and the U.K., among other countries.
Who should not take Tavneos?
Patients with a known serious allergy to the medication or any of its ingredients should not take Tavneos.
The medication also is not recommended for patients with active, untreated, and/or uncontrolled chronic liver disease or serious infections.
How is Tavneos administered in ANCA-associated vasculitis?
Tavneos is available as 10 mg capsules with a yellow body and a light orange cap that’s imprinted with “CCX168” in black ink.
Its recommended dose is 30 mg (three 10 mg capsules), taken twice daily, in the morning and evening, with food. The dosage should be reduced to 30 mg once a day in patients taking medications that strongly suppress the activity of CYP3A4, a liver enzyme that is key for the metabolism of many medications.
The medication should be swallowed whole, and not opened, crushed, or chewed.
Tavneos in clinical trials
The approval of Tavneos was mainly supported by data from a Phase 3 clinical trial called ADVOCATE (NCT02994927).
ADVOCATE
The global ADVOCATE study enrolled 331 GPA or MPA patients at sites across 20 countries. Participants were randomly assigned to receive either Tavneos, at a dose of 30 mg twice daily, or the glucocorticoid prednisone, in addition to standard treatment, for 52 weeks, or about one year. Standard treatment consisted of either cyclophosphamide, followed by azathioprine, or rituximab.
The trial’s main goal was to assess whether Tavneos could replace standard glucocorticoids, such as prednisone, whose long-term use can cause harmful side effects, in AAV treatment.
Specifically, researchers assessed changes in the Birmingham vasculitis activity score, or BVAS, a measure of disease activity. Their aim was to determine if Tavneos was at least as good as prednisone at inducing disease remission at six months, and superior to prednisone at maintaining remission at one year.
Results showed both of these goals were met. Tavneos was associated with a comparable proportion of patients achieving remission at six months relative to prednisone (72.3% vs. 70.1%, respectively), and a significantly higher proportion of patients maintaining remission at one year (65.7% vs. 54.9% in the prednisone group).
Tavneos-treated patients also showed a 54% lower relapse risk at one year, significantly and clinically meaningful improvements in health-related quality of life, and fewer glucocorticoid-related toxic effects compared with those on prednisone, consistent with more glucocorticoids being used in the prednisone group.
Also, Tavneos resulted in significantly greater kidney function improvements in those with severe kidney disease at the study’s start. The therapy’s superiority over prednisone was seen not only at one year, but was sustained for the two months of follow-up after treatment stopped.
Further subgroup analyses showed similar benefits from Tavneos were seen among patients with active ear, nose, or throat (ENT) manifestations, which are common in AAV and negatively affect quality of life.
Ongoing studies
Amgen readied a Phase 3 trial (NCT06321601) for the summer of 2024 to test Tavneos, in combination with standard treatment, in up to 20 children and adolescents, ages 6-17, with active GPA or MPA.
Participants, weighing more than 15 kg, or about 33 lbs., will receive the therapy, along with a rituximab- or cyclophosphamide-containing standard treatment regimen, for one year. Tavneos will be taken twice daily as an oral tablet or liquid formulation.
The trial’s main goals are to assess the proportion of patients reaching and staying in disease remission after six months and after one year. Remission will be evaluated with the Pediatric Vasculitis Activity Score (PVAS), which measures disease activity on a scale from 0 to 63 points, with higher scores indicating more severe disease.
Secondary goals include safety measures, the therapy’s movement into, through, and out of the body, and changes in other measures of disease activity, kidney function, and glucocorticoid dosage.
The study is expected to end in 2030.
Common side effects of Tavneos
The most common side effects of Tavneos include:
- nausea
- headache
- high blood pressure
- diarrhea
- vomiting
- rash
- fatigue
- upper abdominal pain
- dizziness
- increased blood levels of the creatinine molecule, suggesting kidney damage
- numbness, burning, or tingling, usually in the extremities, such as the hands and feet.
Liver damage
Tavneos may cause serious liver damage in some patients. Markers of liver health should be monitored before starting treatment, every four weeks during the first six months on the medication, and as clinically indicated thereafter.
Physicians should proceed with caution if patients develop higher than normal levels of certain liver enzymes suggestive of liver damage. If patients show several signs of liver injury while taking Tavneos, it may be necessary to pause treatment or discontinue it altogether.
Those having signs or symptoms of liver damage, such as yellowing of the skin or the eye’s white part, darkened urine, pain on the upper right side of the abdomen, bleeding, or bruising, should immediately contact their healthcare provider.
The medication should not be taken by patients with cirrhosis or chronic liver disease, such as chronic active hepatitis B. The therapy’s risk-benefit ratio should be considered before giving Tavneos to a patient with liver disease.
Allergic reactions
Treatment with Tavneos may cause allergic reactions, including serious reactions that trigger swelling. This is most common in tissues of the face and throat. The therapy should never be given to anyone with a known allergy to its ingredients.
If an allergic reaction occurs, with symptoms such as swelling of the face, extremities, eyes, lips, tongue, and/or difficulty swallowing or breathing, patients should seek immediate medical attention and treatment should be stopped immediately.
Infections
Because it works by decreasing the activity of a part of the immune system, Tavneos can increase a person’s risk of infections and reduce the ability to fight active or latent infections.
Tavneos may cause serious infections such as pneumonia and urinary tract infections. Therefore, patients should be closely monitored for signs and symptoms of infection during and after Tavneos treatment.
The therapy should not be used in patients with an active, serious infection. Its benefit-risk ratio should be carefully considered before being given to patients with chronic or recurrent infection, a prior history of tuberculosis or a serious or opportunistic infection, or with underlying conditions that make them more prone to infection.
Patients developing signs or symptoms of an infection should immediately contact their healthcare provider.
Cases of hepatitis B virus (HBV) reactivation, including life-threatening hepatitis B, also have been reported with Tavneos. Markers of HBV reactivation should be monitored before initiating treatment.
Patients with evidence of a prior or current hepatitis B virus infection should be seen by a physician with expertise in managing the condition to determine whether HBV antiviral therapy is needed before or during treatment with Tavneos. These patients should be monitored for signs of HBV reactivation or hepatitis during treatment and in the six months thereafter.
If patients develop signs of HBV reactivation while on Tavneos, treatment should be stopped immediately and appropriate antiviral medication should be initiated. Resuming Tavneos should be discussed with physicians with expertise in the matter.
Use in pregnancy and breastfeeding
Tavneos has not been rigorously studied in women who are pregnant or breastfeeding. In animal studies, Tavneos exposure during pregnancy at levels higher than those seen with the therapy’s recommended human dose were associated with some fetal bone abnormalities and an increase in spontaneous abortions, or miscarriages.
Animal studies also have suggested that Tavneos is excreted in breast milk. However, the therapy’s presence in human breast milk and its potential effects on a breastfed infant, or on milk production in nursing patients, remain unknown.
Patients and their healthcare teams should work together to evaluate the potential risks and benefits of Tavneos use by those who are pregnant or breastfeeding.
ANCA Vasculitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Let’s do away with pity parties and start practicing self-compassion
- Urine protein fragments may help assess kidney inflammation in AAV
- Most AAV patients in North America affected by lung complications
- Sharing what’s on your mind can ease loneliness in life with vasculitis
- Antibody type may influence cardiovascular risk timing in AAV
Related articles
-
 Discussion
Discussion
-