Cytokine Levels Can Distinguish Autoantibody Types in AAV Patients, Study Shows
The levels of certain immune molecules called cytokines in the blood are better at identifying the types of specific autoantibodies present in ANCA-associated vasculitis (AAV) patients than at determining clinical diagnosis, a recent study shows.
Based on this finding, researchers suggest that AAV patients should be classified by autoantibody type and not just by their clinical subtype.
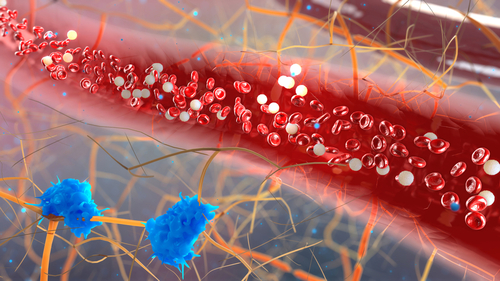
Cytokines help immune cells communicate and trigger immune responses. They are known to play a role in the development of autoimmune diseases, such as AAV. Autoimmunity is characterized by the presence of autoantibodies — which refer to antibodies that attack a person’s own healthy cells. In AAV patients, these autoantibodies are known as antineutrophil cytoplasmic antibodies, or ANCA.
Patients with AAV can be classified into three major subgroups based on their clinical diagnosis: granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA), and microscopic polyangiitis (MPA). However, whether these represent the same disease on a spectrum or three distinct conditions remains a matter of debate.
Though there is often overlap, patients with GPA are more likely to have ANCA directed against a protein called proteinase 3 (PR3), while MPA patients are more likely to have ANCA directed against the protein myeloperoxidase (MPO).
Published in the journal Arthritis & Rheumatology, the study, titled Circulating Cytokine Profiles and ANCA Specificity in Patients with ANCA-Associated Vasculitis,” found that certain cytokine profiles were better at differentiating PR3 and MPO-positive patients than they were at determining patients’ clinical diagnosis, suggesting that the current clinical subtypes are not enough to accurately explain the diversity of the disease.
Recent data suggests that ANCA specificity may actually better predict a number of variables such as response to therapy, relapse risk, and long-term prognosis than the clinical diagnosis of GPA, EGPA, or MPA.
Studies have shown that some cytokines are higher in patients with severe active AAV and decline after treatment. However, no studies until now have looked at cytokine levels across different AAV subtypes.
To address this, researchers sought to characterize the circulating cytokine profiles associated with AAV patients based on ANCA specificity or clinical diagnosis.
Using a panel of 29 cytokines, researchers tested 186 patients with active AAV who took part in the Phase 2/3 RAVE clinical trial (NCT00104299). Researchers then divided these patients according to their ANCA specificity — PR3-AAV or MPO-AAV — as well as a clinical diagnosis of MPA or GPA.
Results showed that levels of nine circulating cytokines — IL-6, GM-CSF, IL-15, IL-18, CXCL8/IL-8, CCL-17/TARC, IL-18BP, sIL-2Ra, NGFb — were significantly higher in patients with PR3-AAV than patients with MPO-AAV.
Another four — sIL6R, sTNFRII, NGAL, sICAM-1 — were significantly higher in patients with MPO-AAV than patients with PR3-AAV.
When classifying patients by their clinical diagnosis, there were six cytokines — IL-6, GM-CSF, IL-15, IL-18, sIL-2Ra, NGFb — that were higher in GPA patients than those with MPA. Additionally, three cytokines — osteopontin, sTNFRII, NGAL — were higher in MPA patients than GPA patients.
Interestingly, for most cytokines, the differences between the PR3-AAV group and the MPO-AAV group were much higher than between the GPA and MPA groups.
Statistical analysis showed that a total of eight cytokines — IL-15, IL-8, IL-18Bp, NGF-b, sICAM-1, TARC, osteopontin, and KIM-1 — were able to differentiate patients better when grouped by ANCA specificity than by their clinical subtype.
“Distinct cytokine profiles were identified for PR3-AAV versus MPO-AAV and for GPA versus MPA. Differences in these circulating immune mediators are more strongly associated with ANCA specificity than with clinical diagnosis, suggesting that the heterogeneity in the AAV subtypes extends beyond the clinical phenotypes,” the researchers concluded.
The investigators believe they “provide additional support for stratification of patients by ANCA specificity for treatment trials.”





