Discussion
Discussion
Abatacept for ANCA-associated vasculitis
Last updated Feb. 21, 2025, by Marisa Wexler, MS

What is abatacept for ANCA-associated vasculitis?
Abatacept is an immunosuppressive therapy that has been explored as a potential strategy to help control disease activity in people with relapsing and non-severe granulomatosis with polyangiitis, or GPA, a common type of ANCA-associated vasculitis.
Administered via subcutaneous, or under-the-skin, injections or directly into the bloodstream (intravenously), the therapy is approved for certain types of arthritis, a condition marked by joint inflammation and pain, and to lower the risk of complications following stem-cell transplant.
Bristol-Myers Squibb markets abatacept for these indications under the brand name Orencia.
Therapy snapshot
| Treatment name: | Abatacept |
| Administration: | Tested in GPA as subcutaneous injections and infusions |
| Clinical testing: | Completed a placebo-controlled Phase 3 clinical trial that failed to meet its main goal; plans for further development are uncertain. |
How does abatacept work in ANCA-associated vasculitis?
ANCA-associated vasculitis, or AAV, is a group of autoimmune diseases characterized by inflammation and damage to small blood vessels, commonly caused by self-targeting antibodies called ANCAs.
GPA, a common AAV type formerly known as Wegener’s granulomatosis, is usually characterized by symptoms affecting the respiratory tract and the kidneys. While immunosuppressive treatments help to maintain disease remission in most GPA patients, relapses are still common.
Several types of immune cells play roles in the inflammatory attack that triggers GPA and drives disease relapses. T-cells, which release pro-inflammatory signaling molecules and may also directly attack a patient’s tissues, are one type of cell that’s centrally involved.
Abatacept is designed to suppress T-cells’ activity. It consists of CTLA4, an immune-regulating protein, fused to part of an antibody that binds to the CD80 and CD86 molecules at the surface of cells that are essential for triggering an immune response from T-cells.
Several changes in CTLA4, CD80, and CD86 levels have been reported in GPA. By binding to CD80 and CD86, abatacept ultimately prevents the cell-cell interaction that triggers T-cells’ activity. By decreasing the inflammatory action of T-cells, abatacept is expected to help reduce disease activity in GPA.
How will abatacept be administered in ANCA-associated vasculitis?
In GPA clinical trials, abatacept was given as monthly intravenous infusions, at a dose of 10 mg/kg, or as weekly subcutaneous injections at a dose of 125 mg.
Abatacept in ANCA-associated vasculitis clinical trials
Abatacept was tested in people with non-severe relapsing GPA in a Phase 1/2 clinical trial (NCT00468208) and in a placebo-controlled Phase 3 study called ABROGATE (NCT02108860).
Phase 1/2 trial
The University of Pennsylvania sponsored a U.S.-based Phase 1/2 trial to assess the safety and efficacy of abatacept in 20 GPA patients, ages 15 and older, who experienced non-severe disease relapses within about a month before entering the study.
All participants were given the therapy via intravenous infusion every other week for the first three infusions, and monthly thereafter. The dose was 10 mg/kg, and treatment continued until the last enrolled patient was treated for six months. Patients were allowed to continue the anti-inflammatory and immunosuppressive medications they were taking when entering the study.
The trial’s main goal was to evaluate abatacept’s safety. Secondary goals included rates of disease remission, disease lessening, and disease relapse, as assessed with the Birmingham Vasculitis Activity Score for Wegener’s Granulomatosis (BVAS/WG).
The results suggested abatacept was generally safe and well tolerated, with the nature, frequency, and severity of the reported adverse events similar to those reported in other GPA trials.
A total of 18 patients (90%) experienced disease lessening, with a BVAS/WG score reduction, while 16 (80%) achieved disease remission — a BVAS/WG score of zero. Disease remission was achieved after about two months of abatacept treatment.
Six participants ended the study early due to disease worsening, including three who had achieved remission but then experienced relapses. The remaining 14 patients stayed in the study through its end, with a median remission time of more than a year.
Prednisone, a glucocorticoid with immunosuppressive properties, was given to 15 patients in the first two months. However, such treatment has been linked to serious side effects when used long-term. Most of these patients (73%) were able to stop taking prednisone, with eight staying off the glucocorticoid through the end of the study.
ABROGATE
The University of South Florida launched the Phase 3 ABROGATE study in 2015 to further test abatacept in non-serious relapsing GPA. The study enrolled 65 patients, ages 15 and older, who had experienced non-serious disease relapses within about a month before study entry.
Participants were randomly assigned to receive a subcutaneous injection of either abatacept (125 mg) or a placebo, once a week, in addition to 30 mg of oral prednisone (or equivalent) per day. The prednisone was tapered and discontinued at week 12, or after about three months. Patients were also allowed to continue their stable immunosuppressive treatments.
ABROGATE’s main goal was to evaluate whether abatacept was better than the placebo at preventing treatment failure over the course of one year. Treatment failure was defined as patients experiencing a relapse or disease worsening, or failing to achieve BVAS/WG of zero (disease remission) or one.
According to trial results presented at scientific meetings in 2024, treatment failure occurred in 62% of abatacept-treated patients and in 68% of those given the placebo. Because differences between the groups did not reach statistical significance, the trial failed to meet its main goal.
Abatacept was also found not significantly superior to the placebo at key secondary goals, including time to remission, duration of glucocorticoid-free remission, relapse severity, and patient-reported quality of life.
Still, the therapy appeared to be well tolerated, with the frequency and severity of adverse events being comparable between the abatacept and placebo groups.
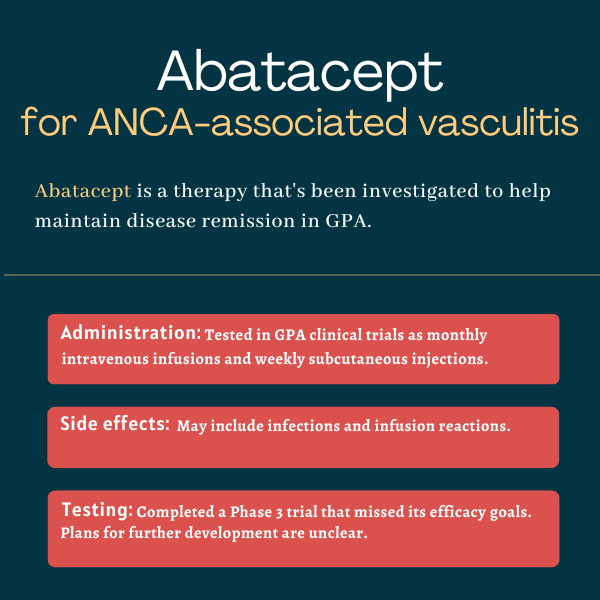
Common side effects of abatacept
In the Phase 1/2 trial of intravenous abatacept in GPA patients, the most commonly reported adverse events related or potentially related to the therapy were infections and infusion-related reactions.
Given that full ABROGATE results have not yet been published, the safety profile of subcutaneous abatacept in people with GPA remains unclear.
Note: ANCA Vasculitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Sharing what’s on your mind can ease loneliness in life with vasculitis
- Antibody type may influence cardiovascular risk timing in AAV
- Tapeworm medication may ease ear, nose, throat symptoms in AAV
- What a hip replacement taught me about bone health and vasculitis
- Cancer risk 23% higher in people with AAV, large US study finds
Related articles
-
 Discussion
Discussion
-