ANCA-associated vasculitis activity, prognosis tied to 2 blood parameters
IL-8 and NLR, two markers of inflammation, are elevated in AAV, studies show
Two blood parameters — interleukin 8 (IL-8) and the neutrophil/lymphocyte ratio (NLR) — may help identify ANCA-associated vasculitis (AAV) patients with high disease activity and those at risk of poor prognosis, a single center study in China suggests.
“IL-18 may be adopted as one of the important biological markers to judge the disease of AAV and … high NLR … may be applied as an indicator to evaluate the poor prognosis,” wrote the researcher in “Detection of serum interleukin-18 level and neutrophil/lymphocyte ratio in patients with antineutrophil cytoplasmic antibody-associated vasculitis and its clinical significance,” which was published in Open Science Training.
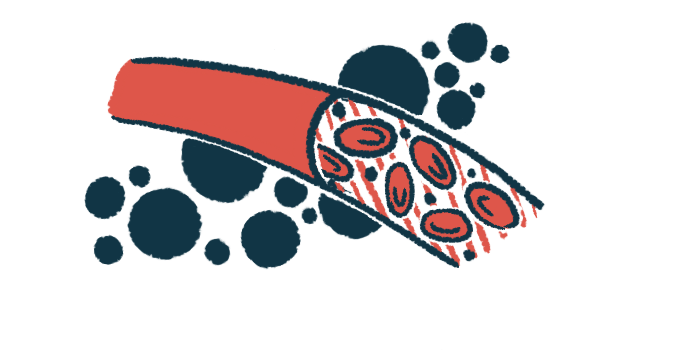
In AAV, the immune system wrongly produces self-targeting antibodies that make blood vessels become inflamed and damaged.
Studies have reported that two markers of inflammation, IL-8 and the NLR, are elevated in AAV patients, supporting their potential use as biomarkers of disease activity. The NLR is a ratio of two types of immune cells.
A researcher at the Liuzhou People’s Hospital, China retrospectively analyzed data from 52 AAV patients (28 men, 24 women; mean age, 54.8) with glomerulonephritis, or inflammation of kidney’s filtering units. They were followed at his hospital between May 2020 and August 2022. Thirty people (mean age, 56.1) with glomerulonephritis not associated with AAV, and 30 healthy volunteers (mean age, 51.3), who served as controls, were also included.
Assessing disease activity, prognosis in ANCA-associated vasculitis
Among AAV patients, 27 had active disease and 25 were in remission, according to the Birmingham vasculitis activity score (BVAS), a measure of AAV activity where higher scores indicate more severe disease. All had kidney involvement and pulmonary involvement was seen in 25 patients (16 with active disease, seven in remission).
Blood levels of creatinine, a marker of kidney damage, were significantly higher in those with active disease than in those in remission (mean 578.43 vs. 231.23 micromol/L). The same was seen for two indicators of inflammation, the erythrocyte sedimentation rate (mean 84.36 vs. 38.64 mm/h) and C-reactive protein (CRP, mean 35.2 vs. 8.73 mg/L).
Circulating levels of IL-18 were higher in AAV patients with active disease than in those in remission and in people with non-AAV glomerulonephritis. Healthy controls and non-AAV glomerulonephritis patients had similar IL-18 levels.
In AAV patients, higher IL-18 levels were significantly associated with higher BVAS scores and ESR levels, indicating higher disease activity and more inflammation.
An IL-8 cutoff value of 136.42 picograms per milliliter assessed AAV activity with a sensitivity of 91.26% and a specificity of 86.7%. A test’s sensitivity is its ability to correctly identify those with a given condition, or active disease, in this case. Specificity refers to correctly identifying those without it, or, in this case, disease remission.
NLR values were significantly higher in AAV patients compared with healthy controls. When the researchers divided the patients based on whether their NLR value was at least 3.77 or not, they found BVAS scores were significantly increased in the high NLR group (mean 12.43 vs 17.52).
The same was seen for other blood parameters indicating higher inflammation, including white blood cell count, absolute neutrophil count, and CRP levels.
Also, estimated glomerular filtration rate, a measure of kidney function, was significantly lower in the high NLR group relative to the low NLR group (mean 76.19 vs. 14.87 mL/min/1.73m2).
A significantly lower proportion of patients in the low NLR group received treatment with steroid pulses relative to those in the high NLR group (22.22% vs. 64%). Other treatment regimens had no obvious distinction between the two groups.
The four-year cumulative survival rate, or the proportion of patients who survived over that period, was significantly higher in the low NLR group than in the high NLR group (68.36 vs. 42.89%).
The findings “confirmed that IL-18 was correlated with AAV activity and could be used as a marker to assess AAV activity,” the researcher wrote, while “high NLR can be applied as one of the important indicators of poor prognosis.”