Immune Cell Ratio Can Help Identify Patients at High Risk of Infection
A higher ratio of disease-inducing neutrophils to lymphocytes at diagnosis may help predict severe infections and mortality in people with ANCA-associated vasculitis (AAV) taking immunosuppression therapy, a study suggests.
The study, “The neutrophil-to-lymphocyte ratio as a marker of vasculitis activity, severe infection and mortality in anca-associated vasculitis,” was published in the journal Nefrología.
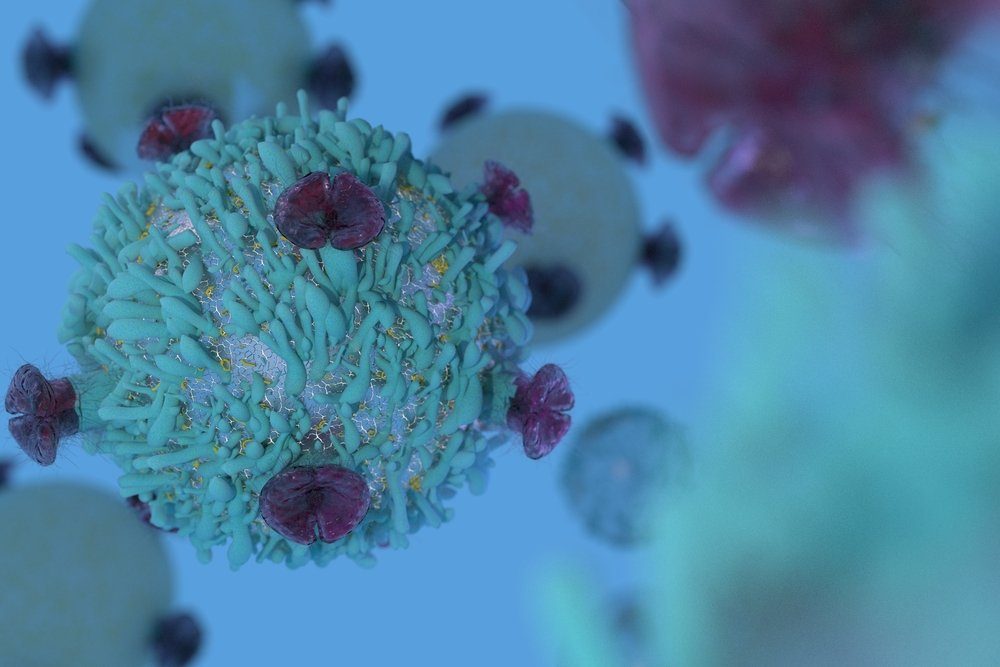
AAV is an autoimmune disease in which the immune system attacks and damages blood vessels. This happens because the body erroneously produces autoantibodies (self antibodies) that activate immune cells called neutrophils that attack blood vessels.
The disease is typically treated with immunosuppressants, which have dramatically improved patient short-term prognoses and reduced mortality rates. However, the long-term outcomes and adverse effects of these treatments in AAV patients have not been well-explored.
The neutrophil-lymphocyte ratio (NLR), the ratio of neutrophils to another immune cell type called lymphocytes, is a biomarker of systemic inflammation that has been used to predict patient prognosis for cancers and kidney failure, among other conditions.
Thus, researchers at a nephrology and renal transplant center in Lisbon, Portugal, sought to determine if NLR could similarly predict the risk of severe infection and mortality in AAV patients within one year of diagnosis.
Retrospective health data from adults with AVV were collected from 2006 to 2019. Clinical data at diagnosis were assessed, along with severe infection three months after diagnosis and mortality after one year.
The study included 45 patients with a mean age of 67.5 at diagnosis, of which 51.1% were male and 97.8% were white. A total of 36 patients (80%) had rapidly progressive kidney failure, 25 (55.6%) required kidney dialysis, and 13 (28.9%) experienced bleeding in the lungs.
The researchers assessed the blood levels of several disease markers. The mean levels of creatinine, a marker of kidney function, and hemoglobin, an oxygen-carrying protein in red blood cells, were well below the normal range. In contrast, markers of systemic inflammation were above the normal range.
Patients received a variety of immunosuppressant therapies, including cyclophosphamide (35 patients), corticosteroids (35 patients), and rituximab (8 patients). One-third of patients underwent plasma exchange, which consists of replacing the liquid part of blood to eliminate autoantibodies in circulation.
Following immunosuppression, two-thirds (66.7%) of patients recovered kidney function at discharge and 64.4% continued therapy after discharge. In the three months following treatment, 20 patients (44.4%) developed severe infections, and 10 (22.2%) experienced a reduction of white blood cells.
The patients who developed severe infections were older, with a mean age of 73.6 years compared to 62.6 years in patients without severe infections. Moreover, these patients had a higher incidence of lung bleeding, and higher NLR at admission.
Rituximab treatment was associated with fewer severe infections than other treatments (5% vs. 28%). Older age and higher NLR at diagnosis were found to be the best predictors of severe infection within three months of treatment.
Notably, an NLR of 4.04 or above predicted severe infection within three months of treatment with 95% sensitivity (5% false-negatives) and 52% specificity (48% false-positives).
Nine patients (20%) died within one year of diagnosis. These patients were older (mean age of 76.8 years vs. 65.2 years), and more often developed a severe infection (77.8% vs. 36.1%), indicating that older age and severe infection were both associated with a greater mortality risk.
Based on these results, the investigators suggest that NLR is a biomarker for AAV patient outcomes.
“This ratio can be quickly assessed from a routine blood sample and can prove useful in identifying patients at risk of infection. Recognizing high risk patients is crucial to guide immunosuppression and improve patient outcomes,” they wrote.
Among the study limitations is the small, retrospective, and single-center nature of the study, potential overestimation of association between NLR and age due to lack of age-adjusted NLR analysis, and lack of data on infection source and cause of mortality.
“We highlight the need for further understanding of AAV in order to identify at-risk patients, guide immunosuppression and ultimately improve patient outcomes,” the team concluded.