Prednisolone Dose, Poorer Kidney Health Linked to Severe COVID-19
AAV patients with severe infection on higher daily immunosuppressive dose
Written by |
Poorer kidney function and relatively high doses of the corticosteroid prednisolone — possibly indicating active disease — can increase the risk of severe COVID-19 for people with ANCA-associated vasculitis (AAV), a Swedish study suggests.
“Our findings highlight risks and suggest that more attention should be given to optimal AAV treatment in a pandemic situation,” its researchers wrote.
The study, “Risks and treatment related aspects of COVID-19 infection in patients with ANCA-associated vasculitis,” was published as a brief report in the Scandinavian Journal of Rheumatology.
AAV occurs when the immune system wrongly attacks small blood vessels in the body, causing them to become inflamed. Its treatment involves immunosuppressants, medications to ease inflammation. They can be used to push the disease into remission, where no symptoms appear for a time, and to maintain remission.
Immunosuppressants work by toning down the immune system and keeping its actions in check. These treatments for AAV include prednisolone, cyclophosphamide (sold as Cytoxan, among other names), and rituximab (sold as Rituxan in the U.S., MabThera in Europe, and available as biosimilars).
But at higher doses taken for longer periods, immunosuppressants can weaken the immune system to a point where the body fails to mount a response fit enough to fight off infections and other diseases. When this happens, patients are said to be immunocompromised.
Higher median daily prednisolone doses in those with severe COVID-19
This was particularly important during the COVID-19 pandemic, since an immunocompromised person is more likely to contract COVID-19 and become severely ill. Those who are immunocompromised are also more likely to fail to respond to vaccination and not be protected, even if they stay up to date with their vaccines.
While taking corticosteroids or other immunosuppressants is thought to put AAV patients at higher risk of severe COVID-19, more data are needed to determine what additional precautions may be necessary.
A team led by Karolinska Institutet researchers drew on data covering 310 AAV patients with medical records available from March 2020 to January or May 2021, treated at Karolinska University Hospital in Stockholm and Uppsala University Hospital. The group included 157 women and 153 men with a median age of 67.
By AAV type, 232 patients (74.8%) had granulomatosis with polyangiitis, 56 (18.1%) had microscopic polyangiitis, and 22 (7.1%) had eosinophilic granulomatosis with polyangiitis. The majority (94.8%) tested positive for ANCAs, the autoantibodies that typically drive AAV.
Over the course of the study, 29 patients (9.4%) were diagnosed COVID-19. These people had AAV for median of 118 months (almost 10 years) and were generally eight years younger than those not diagnosed with COVID-19 (median of 60 vs. 68 years).
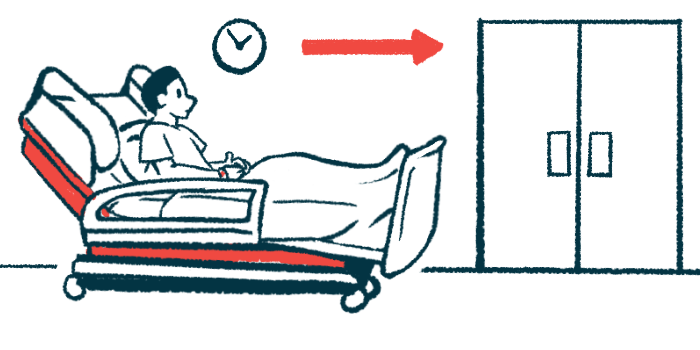
Nine of the 29 patients (31%) — four women and five men — developed severe COVID-19, requiring noninvasive ventilation to help them breathe or admission to an intensive care unit. Four of them (13.8%) died of COVID-19 complications within one month.
About the same proportion of patients with or without COVID-19 were receiving treatment with prednisolone (51.7% vs. 46.3%). However, those with COVID-19 were taking significantly higher median daily doses (6.25 vs. 5 mg/day), with their maximum daily dose reaching up to 50 mg.
Other disease-modifying medications were used by about the same proportion of patients with or without COVID-19 (65.5% vs. 64.8%). Induction therapy with cyclophosphamide and rituximab — used alone or in combination — was more common in patients with COVID-19 than without it (13.8% vs. 2.5%).
Between patients with or without severe COVID-19, prednisolone’s use was almost twice as common in those with severe illness relative to patients with a milder infection (77.8% vs. 40%). Moreover, the median daily dose of prednisolone was 50% higher in those with severe illness (7.5 mg/day; range, 5–50 mg daily) than among those without (5 mg/day; range of 2.5–5 mg).
Maintenance therapy not linked to severe COVID-19 course
However, about the same proportion of severe and non-severe COVID-19 patients were on induction or maintenance therapy with cyclophosphamide or rituximab, a finding that may calm concerns of rituximab posing an added COVID risk.
“Maintenance therapy was not associated with a more severe disease course suggests that adjusting immunosuppressive therapy is important when clinically possible,” the researchers wrote.
Severe COVID-19 patients had poorer kidney function prior to infection than those with a milder infection, as seen by a lower median estimated glomerular filtration rate (eGFR), a measure of how well the kidneys are working.
“Risk factors for severe COVID-19 were impaired kidney function [and] more intense immunosuppressive therapy, which may also reflect an active AAV disease state as a potential risk,” the researchers wrote.
These findings “emphasize the need for continued shielding, mitigation strategies, and effective vaccination of AAV patients,” they added.






