Risk of hip joint collapse in AAV linked to prednisolone: Study
Decreasing glucocorticoids 90 days after RIT, early detection important for intervention
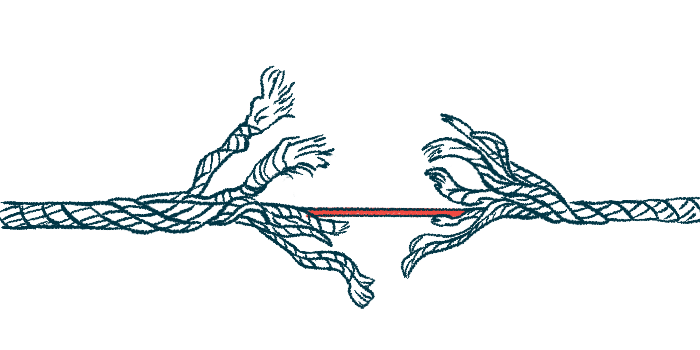
Nearly one-fifth of ANCA-associated vasculitis (AAV) patients in Japan have osteonecrosis of the femoral head (ONFH), a condition marked by the disruption of blood flow to the head of the femur, or thigh bone, a study showed.
In most cases, the hip joints already collapsed or were at risk of a collapse. Also, a higher daily dose of prednisolone, a standard immunosuppressive AAV treatment, by day 90 of initial remission induction therapy (RIT) was identified as an independent ONFH risk factor.
“A rapid reduction of glucocorticoids in 90 days after RIT and early detection of pre-collapse ONFH by MRI screening are important for decreasing and intervening ONFH development in AAV patients,” the researchers wrote in the study, “Prevalence and risk factors of osteonecrosis of the femoral head in patients with ANCA-associated vasculitis: a multicenter cohort study,” which was published in RMD Open.
AAV is driven by the production of self-reactive antibodies, called ANCAs, that cause inflammation and damage to the body’s small blood vessels. The disease is also marked by the presence of neutrophil extracellular traps (NETs), specific structures formed by neutrophils, a type of immune cell.
NETs normally work as a web that traps and kills disease-causing microbes, but can also release molecules that contribute to autoimmunity and tissue damage.
Standard remission-induction therapy in AAV usually combines glucocorticoids such as prednisolone and either rituximab or cyclophosphamide to reduce inflammation and immune responses. Rituximab is sold as Rituxan in the U.S. and MabThera in Europe, with biosimilars available.
Previous studies have identified NETs, blood vessel inflammation, and glucocorticoid use as risk factors of ONFH, which “causes collapse of the femoral head and dysfunction of the hip joint, resulting in a decline in the quality of life,” the researchers wrote.
The prevalence and risk factors of ONFH in people with AAV remains unknown, however, leading researchers in Japan to retrospectively analyze data from 186 patients diagnosed at the Chiba University Hospital and 11 affiliated hospitals between March 2007 and April 2021.
Role of prednisolone in hip joint collapse assessed
None had any hip symptoms at the time of their diagnosis and all agreed to radiographs and a MRI of both hip joints after six months after initiating RIT with prednisolone.
The patients’ median age at the onset of AAV was 70.5 and hip joint MRI screening for ONFH was performed at a median of 2.6 years after diagnosis.
The results showed 33 patients (17.7%) had ONFH and the condition affected both hip joints in 63.6% of them. More than half (54.5%) of patients diagnosed with ONFH had no symptoms.
Ten patients showed evidence of hip joint tissue breakdown, but none had hip pain at their diagnosis.
The researchers found no significant differences between those who developed ONFH and those who didn’t in terms of AAV features, known ONFH risk factors such as alcohol consumption and history of smoking, or known risk factors of blood flow interruption.
A total of 33 AAV patients with ONFH had signs of bone tissue death in 54 femoral head joints, with most (75.9%) being in pre-collapse stages. The remaining 13 joints (24.1%) were already collapsed. More than half (56.1%) of the pre-collapse stage joints were at risk of collapse.
As such, “two-thirds of the ONFH joints were already in collapse stages or at risk of future collapse in our radiographs and MRI screening,” the researchers wrote.
Even in the asymptomatic patients, almost all hip joints (96.6%) were in pre-collapse stages, with more than one-third (39.3%) being at risk of future collapse.
Hip pain after RIT
The presence of ONFH with collapsed hip joints or joints at risk of future collapse was significantly associated with developing hip pain after starting RIT.
Regarding RIT, all patients received prednisolone, at a median initial dose of 40 mg/day. A total of 35 patients (18.8%) were given methylprednisolone pulse therapy.
A dose of 20 mg/day or higher by day 90 of RIT, was a significant, independent risk factor of ONFH in AAV patients, statistical analyses showed.
Rituximab appeared to be linked to a reduced ONFH risk, but this association failed to reach statistical significance. However, the prednisolone dose by day 90 was significantly lower in rituximab-treated patients than in those without it (mean, 14 vs. 20 mg/day).
Overall, “we have shown that 18% of AAV patients develop ONFH after RIT and that glucocorticoid dose on day 90 of RIT is an independent risk factor for ONFH in AAV patients,” the researchers wrote. “Our results suggest that the combination of lower doses of glucocorticoids and rituximab would be useful in preventing or slowing the progression of ONFH in AAV patients.”
The researchers said the best times for MRI screening (e.g., six months and 12 months after RIT) to find the “pre-collapse ONFH in high-risk patients should be determined in a future prospective longitudinal study.”