Fasenra (benralizumab) for ANCA-associated vasculitis
Last updated Oct. 31, 2024, by Marta Figueiredo, PhD

What is Fasenra for ANCA-associated vasculitis?
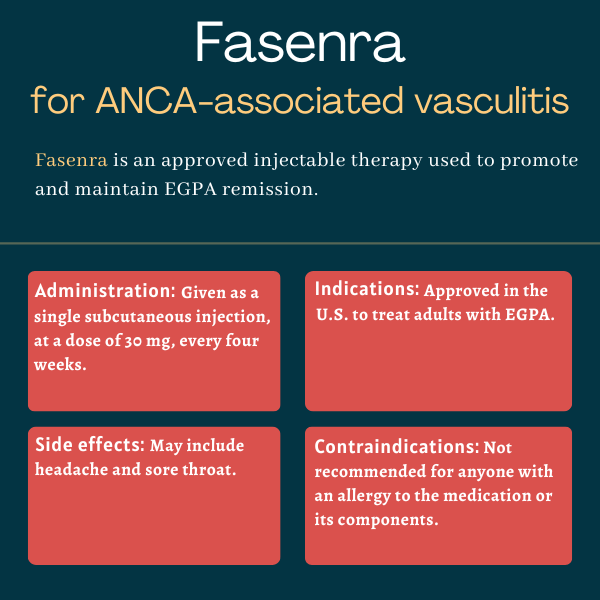
Fasenra (benralizumab) is an approved therapy for adults with eosinophilic granulomatosis with polyangiitis (EGPA), a rare form of ANCA-associated vasculitis (AAV).
Administered through under-the-skin, or subcutaneous, injections, the therapy is expected to promote and maintain disease remission, while also reducing the need for standard glucocorticoids, whose long-term use is linked to serious side effects.
Fasenra was developed by AstraZeneca and its global biologics research and development arm MedImmune. It is also approved for treating severe eosinophilic asthma, a rare type of asthma associated with similar immune-related mechanisms.
Therapy snapshot
| Brand name: | Fasenra |
| Chemical name: | Benralizumab |
| Usage: | Used to treat adults with EGPA; can help promote and maintain disease remission |
| Administration: | Subcutaneous injection |
How does Fasenra work?
Like other types of ANCA-associated vasculitis, EGPA is an autoimmune disease marked by damaging inflammation in small blood vessels that can affect the function of several organs and tissues.
In EGPA, the rarest AAV type, small clumps of eosinophils, a type of immune cell, build up in small blood vessels and nearly all patients have very high counts of eosinophils at some point in their disease course. Eosinophils normally defend the body against parasites, bacteria, and viruses, but can also cause damage as part of the inflammatory responses triggered by allergies.
The disease causes symptoms that most often affect the respiratory tract, leading to asthma in more than 90% of cases, and the gastrointestinal tract.
The mainstay treatment for EGPA consists of anti-inflammatory oral medications called glucocorticoids. High doses of and/or long-term treatment with glucocorticoids can result in serious side effects such as high blood pressure, diabetes, weight gain, and sleep and mental health problems, however.
Fasenra, formerly MEDI-563, is an antibody-based therapy designed to bind and prevent the activation of IL-5 receptor alpha (IL-5R-alpha), a protein activated by IL-5 and found almost exclusively on the surface of eosinophils. IL-5/IL-5R-alpha signaling is essential for the growth, activation, and survival of eosinophils.
Fasenra blocks this signaling and also causes the death of eosinophils by boosting the binding of other immune cells to Fasenra-covered eosinophils and their precursors, promoting their death.
As such, the therapy is expected to limit disease-driving inflammation, promote disease remission, and reduce risk of relapse in people with EGPA.
Fasenra’s mechanism of action is similar to that of GSK’s Nucala (mepolizumab), which is approved for EGPA as an add-on to glucocorticoids. Nucala, given as three separate subcutaneous injections every four weeks, is an antibody-based therapy that promotes eosinophil death only indirectly by targeting IL-5.
Who can take Fasenra?
The U.S. Food and Drug Administration approved Fasenra to treat adults with EGPA in September 2024. The decision marked the second approved therapy for the condition, and the first to involve a single injection, once a month. About a month later, the therapy was approved in the European Union for adults with relapsing or treatment-resistant EGPA.
Who should not take Fasenra?
Fasenra should not be taken by anyone with a known allergy to the medication or any of its ingredients.
How is Fasenra administered in ANCA-associated vasculitis?
For people with EGPA, Fasenra is administered at a recommended dose of 30 mg, via a single subcutaneous injection once every four weeks.
The therapy is available as a single-dose prefilled syringe and a single-dose prefilled autoinjector pen, each containing 30 mg of the therapy in 1 mL of liquid that is clear to opalescent in sheen, and colorless to yellowish in color. The liquid may also contain a few particles that may be translucent or white to off-white in color.
The prefilled syringe is meant to be used by healthcare providers, while the autoinjector pen can be used by patients themselves and their caregivers after appropriate training by a healthcare provider.
Before administration, the prefilled autoinjector should be removed from the refrigerator and allowed to warm at room temperature for about 30 minutes. No other warming methods should be used. If needed, Fasenra can be stored at room temperature for up to 14 days.
Fasenra injections may be given into the front of the thighs or the lower part of the stomach area — but not within 2 inches (about 5 cm) of the belly button. The upper arm can be used as an injection site if the therapy is administered by a caregiver or a healthcare professional. Each injection should be given at least 1 inch (about 2.5 cm) away from the last injection site.
The injection site — which should not be tender, bruised, scarred, scaly, damaged, or hard — should first be disinfected. The autoinjector should be held against the skin at a 90-degree angle for up to 15 seconds after the start of the injection.
If a planned dose of Fasenra is missed, patients should call their healthcare provider.
Fasenra in clinical trials
Fasenra’s approval for EGPA was mainly based on results from a global head-to-head Phase 3 clinical trial, called MANDARA (NCT04157348), to evaluate Fasenra’s safety and effectiveness against Nucala in 140 adults with difficult-to-treat EGPA.
MANDARA
All patients had relapsed at more than three months, but less than two years, before enrolling; had failed to achieve disease remission following standard induction regimen; or had symptom recurrence upon oral glucocorticoid tapering at doses of at least 7.5 mg per day.
The participants, who all were receiving stable doses of oral glucocorticoids with or without stable immunosuppressive treatment, were randomly assigned to Fasenra or Nucala for about a year.
Fasenra was given as one 30 mg injection every four weeks and Nucala as three 100 mg injections every four weeks. Patients could continue their standard-of-care treatment, and oral glucocorticoids could be tapered from week 4 onward, at the discretion of the investigator.
The study’s main goal was to determine if Fasenra was at least not inferior to Nucala at inducing disease remission at both weeks 36 and 48. This was assessed through the proportion of patients who achieved remission, defined as a Birmingham Vasculitis Activity Score of zero (no symptoms) while taking 4 mg/day or less of oral glucocorticoids.
Secondary goals included remission duration, time to first relapse, relapse rates, changes in disease severity and activity, and the proportion of patients able to reduce their corticosteroid dose. Other measures included side effects and the number of hospitalizations and emergency care visits related to EGPA.
Top-line results, announced in 2023, showed remission rates were comparable between treatment groups: 59% with Fasenra and 57% with Nucala.
Secondary measures also supported that Fasenra was not inferior to Nucala. Specifically, no significant differences were seen regarding remission duration, the proportion of patients in remission within six months who stayed in remission to a year (42% vs. 37%), and relapse rates (30% in both groups).
In the last four weeks of treatment, a higher proportion of Fasenra-treated patients reduced their oral glucocorticoid dose by at least 50% (86% vs. 74%) and were able to fully taper off these medications (41% vs. 26%).
Moreover, Fasenra treatment was associated with greater reductions in blood eosinophil counts, starting as early as the first week and sustained through a year of treatment.
Safety data from both therapies were comparable.
Those who completed the one-year treatment could choose to move into the trial’s open-label extension phase, where all receive Fasenra for at least one year.
Ongoing trials
AstraZeneca also launched an international Phase 3 trial, called CLIPS (NCT06512883), to evaluate Fasenra’s safety, tolerability, efficacy, and pharmacological properties in children, ages 6-17 years, with rare conditions marked by high levels of eosinophils.
The first group of 14 patients will include EGPA pediatric patients on stable oral glucocorticoids, with or without immunosuppressive treatments. All will receive a weight-based dose of Fasenra, once a month, for up to one year.
CLIPS’ main goals are to assess rates of adverse events and changes in the levels of the medication in the blood. Secondary goals include the proportion of EGPA patients achieving disease remission after six months and time to first relapse. Changes in eosinophil counts will also be assessed, as will the presence of antibodies against the therapy.
Those completing the one-year treatment period may enter the study’s extension period, where all will receive Fasenra for another year.
The trial is set to end in 2027.
Common side effects of Fasenra
The most common side effects of Fasenra in people with EGPA include:
- headache
- sore throat.
Allergic reactions
Fasenra may cause allergic reactions within hours or days after dosing. Symptoms may include swelling of the face, mouth, and/or tongue; breathing difficulties; low blood pressure that can lead to dizziness or lightheadedness, and fainting; rash; and hives.
If an allergic reaction occurs, patients should immediately inform their healthcare provider or get medical help, and permanently discontinue Fasenra treatment.
Acute asthma symptoms or exacerbations
Fasenra should not be used to manage acute symptoms or sudden symptom worsening (exacerbations) of asthma. If asthma remains uncontrolled or if it worsens after initiating Fasenra treatment, patients should seek medical advice.
Considerations for reducing glucocorticoids
While Fasenra has been shown to reduce the need for glucocorticoids, patients should not abruptly stop these medications, as this can lead to withdrawal symptoms and/or reveal health conditions that were being controlled by glucocorticoids. As such, if glucocorticoid dosage needs to be reduced, this should be done gradually under the supervision of a physician.
Parasitic infections
Due to the therapy’s suppressing effects on eosinophils, which may be involved in the fight against some helminths, or parasitic worms, people on Fasenra may be at a higher risk of parasitic infections.
Patients with known parasitic worm infections were excluded from Fasenra trials, so it is unknown whether the therapy impairs these patients’ immune response to such infections.
Those with preexisting helminth infections should receive appropriate treatment for the parasite before initiating treatment with Fasenra. If patients develop a parasitic worm infection while on Fasenra and do not respond to appropriate treatment, Fasenra should be withheld until the parasitic infection resolves.
Use in pregnancy and breastfeeding
Fasenra has not been rigorously studied in people who are pregnant or breastfeeding. In monkey studies, there were no signs of fetal harm when Fasenra was given during pregnancy at doses up to 310 times the maximum recommended dose for people.
The therapy’s presence in human breast milk and its potential effects on a breastfed infant, or on milk production in nursing patients, also remain unclear.
Patients should work together with their healthcare teams to evaluate the potential risks and benefits of Fasenra use by those who are pregnant or breastfeeding.
Note: ANCA Vasculitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Tapeworm medication may ease ear, nose, throat symptoms in AAV
- What a hip replacement taught me about bone health and vasculitis
- Cancer risk 23% higher in people with AAV, large US study finds
- Asthma drug dupilumab may ease symptoms in EGPA: Small study
- A valentine for the people who show up in our lives with ANCA vasculitis