Complement System Activation May Be Linked to Kidney Disease in AAV Patients
Written by |
The complement system, a component of the immune system, is overactive in people with necrotizing glomerulonephritis, or inflammation in the tiny blood vessels of the kidneys, caused by ANCA-associated vasculitis (AAV), a study reports.
Some complement proteins seem to correlate with more severe kidney disease in these patients, and may be used to predict patient outcomes.
The study, “Systemic complement activation in anti‐neutrophil cytoplasmic antibody‐ associated vasculitis and necrotizing glomerulonephritis,” was published in Nephrology.
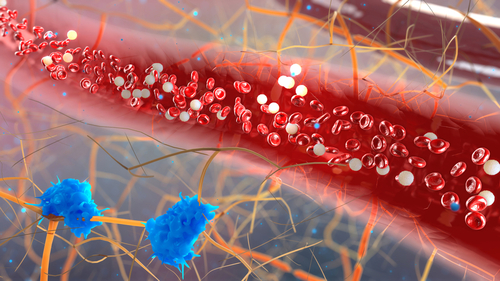
The complement system is a group of more than 20 immune proteins that are found in blood and tissue fluids. Normally, these proteins are present in an inactive state, but in response to certain signals (e.g., infectious bacteria), the proteins are activated, most prominently through cleavage. The activated proteins trigger increased inflammation.
While the complement system has not historically been thought to play a significant role in AAV, recent evidence has suggested that this system could be overactivated in people with AAV. Additionally, animal models have shown that necrotizing glomerulonephritis cannot develop without certain complement proteins.
Researchers in Greece set out to examine levels of activated complement proteins in the blood of 56 people with AAV and necrotizing glomerulonephritis, aiming to establish their correlation with disease activity and outcomes.
For comparison, complement activation was also measured in 20 people without AAV who were used as controls. The two groups were similar in terms of age, sex, and race.
Most of the patients (73.2%) had antibodies against the proteinase 3 or myeloperoxidase proteins, and significant impairment of kidney function — half required urgent hemodialysis at presentation.
The complement components measured included complement 5a (C5a), complement Bb fragment (Bb), complement 3a, and complement 4d, and all were significantly higher in people with AAV than in controls. These results indicate overactivation throughout the complement system in people with AAV.
Among those with AAV, the levels of many individual complement components were significantly correlated. For instance, people with AAV who had higher Bb levels were statistically more likely to also have higher levels of C5a, C3a, and C4d.
Additionally, there were strong correlations between C5a and Bb levels and poor kidney function at diagnosis. In fact, patients requiring hemodialysis had significantly higher levels of both C5a and Bb than those with preserved kidney function.
“An interesting question arising at this point is whether renal function impairment is the result or the cause of increased C5a and Bb levels,” the researchers wrote, suggesting an area for future investigation.
With two years of follow-up, during which time people with AAV were given standard treatments, there were no significant correlations between complement component levels at the time of diagnosis and long-term kidney function.
“We found that C5a and Bb levels had significant negative correlation with renal function at time of renal biopsy, and this correlation remained strong during the acute phase of the disease,” the researchers wrote.
But “after two years follow up, this correlation disappeared, suggesting that immunological and inflammatory pathways, including activation of complement, are successfully regulated by immunosuppressive treatment, which can affect their production and their impact of renal disease,” they added.
These findings add to the growing body of research implicating complement activation in AAV. Further understanding the role this system plays could open avenues for better monitoring or treatment of AAV.
“C5a and Bb complement fragments seem to play a critical role in the induction of the disease, and could possibly both be used as biomarkers to predict disease activity and renal function outcome,” the researchers wrote.





