Lower glucocorticoid dose effective for AAV with kidney issues: Study
It results in similar outcomes as higher-dose option, may lower infection risk
Written by |
A low-dose course of glucocorticoid therapy results in similar outcomes as a higher-dose option in people with ANCA-associated vasculitis (AAV) and kidney involvement, though it may lower risk of serious infection, a study reports.
“Our findings reinforce the safety and efficacy of reduced [glucocorticoid] as the initial [glucocorticoid] regimen of choice for patients with severe kidney involvement,” the research team wrote. This supports the real-world application of results from a clinical trial, which demonstrated similar efficacy for low- and high-dose plans.
Although lowering the glucocorticoid dose didn’t significantly impact outcomes in the study population, rates of serious complications were still common. Researchers highlight the need for more effective treatment options for people with severe kidney problems linked to AAV.
The study, “Glucocorticoid dosing and outcomes in ANCA-associated vasculitis with kidney involvement,” was published in Kidney International Reports.
Biopsy confirms diagnosis of AAV with kidney involvement
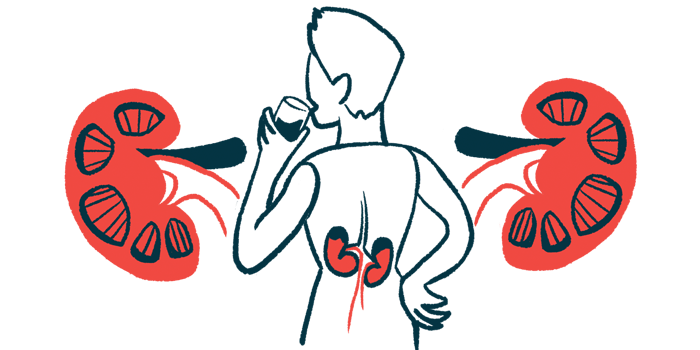
In AAV, a group of autoimmune conditions, immune cells mistakenly attack the lining of small blood vessels, causing inflammation and damage. Symptoms largely depend on which organs and tissues are impacted.
Kidney damage is a common manifestation of AAV, and this may lead to chronic kidney disease and kidney failure.
Cyclophosphamide and rituximab (sold as Rituxan in the U.S. and Japan, with available biosimilars) often play a role in the treatment of AAV with organ involvement. These are typically administered alongside glucocorticoids such as prednisone, which can ease inflammation. However, glucocorticoids also suppress immune system function, potentially leaving patients vulnerable to infection.
Because of this risk, there has been increasing interest in reducing dosage of glucocorticoids. The PEXIVAS clinical trial (NCT00987389) found similar outcomes for reduced-dose and standard-dose regimens. This finding prompted clinicians to adopt lower-dose models in their practice.
Despite this, “real-world studies show that clinicians may be reluctant to use reduced-dose [glucocorticoid] regimens for AAV, particularly for organ- or life-threatening disease,” the researchers wrote.
This study focused on The Ottawa Hospital in Canada. In 2020, kidney specialists at the hospital adopted reduced glucocorticoid dosing as the norm for their AAV patients. The researchers examined clinical records for 97 individuals treated at the hospital before this shift, which they termed the standard-glucocorticoid era, and 41 treated after, dubbed the reduced-dose era. All had undergone kidney biopsy to confirm a diagnosis of AAV with kidney involvement.
Generally, the reduced-dose era group was older at the time of biopsy (mean age of 70.3 vs. 63.1). Starting kidney function was poorer in the reduced-dose era group.
Most participants received glucocorticoids alongside cyclophosphamide and/or rituximab. In the standard-dose era, cyclophosphamide was most common (78.4%). The reduced-dose era group had a more even split between the two medications when used alone.
Remission rates similar between standard-, reduced-dose groups
The team assessed the proportion of each group that died or developed end-stage kidney disease within the first year after biopsy. There was no significant difference, with 24.4% of the reduced-dose era group and 21.6% of the standard-dose era group experiencing one of these outcomes.
Rates of remission within six months were also similar, with about 63% to 64% of each group reaching this status. There also weren’t significant differences in risk of serious infection or change in kidney function metrics.
The team then divided the participants based on each person’s cumulative dose of prednisone in the first month of treatment.
To improve patient outcomes and reduce treatment-related complications, future studies should explore strategies to further reduce [glucocorticoid] exposure, reduce rates of infection and improve kidney function recovery.
People in the lowest dosage group tended to have the lowest risk of serious infection. However, they had a higher risk of death or end-stage kidney disease relative to the highest dosage group.
“This highlights the importance of finding [glucocorticoid]-sparing induction regimens that could minimise [glucocorticoid] use in patients with severe kidney involvement, without reducing treatment efficacy,” the researchers wrote.
Noting the relatively high rate of death and end-stage kidney disease across all participants, the team also highlighted the need for other interventions to improve kidney function in this population.
Among the factors that may have limited the study, the team noted that the COVID-19 pandemic may have delayed access to in-person medical care in the reduced-dose era.
“To improve patient outcomes and reduce treatment-related complications, future studies should explore strategies to further reduce [glucocorticoid] exposure, reduce rates of infection, and improve kidney function recovery,” the scientists wrote.