GPA and EGPA overlap features linked to disease severity, survival risk: Study
Distinctions between groups could have implications for treatment strategies
Written by |
People with overlapping features of granulomatosis with polyangiitis (GPA) and eosinophilic granulomatosis with polyangiitis (EGPA), two types of ANCA-associated vasculitis, may exhibit distinct disease characteristics that influence disease severity and prognosis, a study reveals.
By analyzing data from more than 100 people with overlapping GPA/EGPA features, a team of researchers in Europe identified three overlapping disease groups based on organ involvement and clinical outcomes.
One group overlapping equally with both EGPA and GPA had better survival, while the other two groups — one with greater body-wide involvement and another with more severe disease — aligned more closely with typical GPA and had poorer survival rates.
“These distinctions have important clinical implications, particularly for optimizing treatment strategies tailored to individual patient profiles,” researchers wrote.
The study, “Overlapping forms of granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis: Insights from a European multicenter study,” was published in the Journal of Internal Medicine.
GPA and EGPA both characterized by presence of granulomas
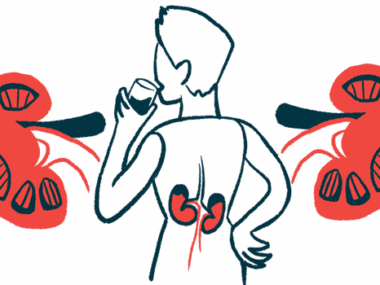
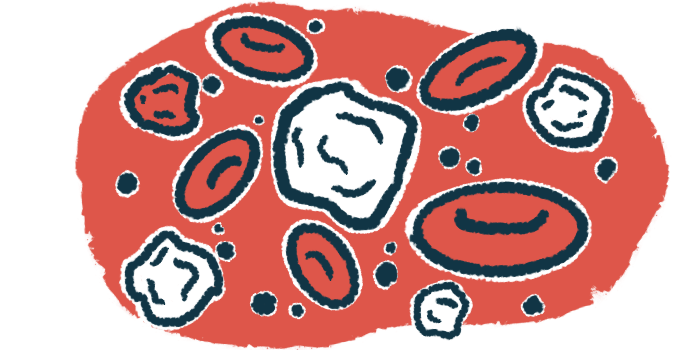
ANCA-associated vasculitis refers to a group of autoimmune diseases characterized by inflammation and damage to small blood vessels, typically caused by self-reactive antibodies known as ANCAs. GPA is one of the two most common types of the disease, while EGPA is the rarest type.
Both GPA and EGPA are characterized by the presence of masses of immune cells, called granulomas, that in EGPA are primarily made of eosinophils. GPA typically affects the kidneys and respiratory tract, while EGPA most commonly affects the lungs, heart, and gastrointestinal tract.
Most people with GPA have ANCAs against the proteinase 3 (PR3) protein, while “only 30%–40% of EGPA patients are ANCA-positive, primarily [targeting the MPO protein], with PR3-ANCA being rare (1%–3%),” the researchers wrote.
However, cases of overlapping features between GPA and EGPA are being increasingly recognized, raising questions regarding disease management, as therapeutic approaches differ significantly between these two types.
To gain a deeper understanding, a team of international researchers analyzed data from 135 adults with overlapping GPA and EGPA features who were followed at multiple centers across eight European countries. Participants were primarily men (62.2%) and had a mean age of 52.5 years at the time of diagnosis.
Lung problems most frequent symptom of study participants
The most frequent symptoms were lung problems (90.4%), followed by ear, nose, and throat (ENT) involvement (84.4%). Rounding out the list were skin (51.9%), kidney (47.4%), peripheral nerve (40%), and cardiovascular involvement (23%). Peripheral nerves are those found outside the brain and spinal cord.
Three groups of patients were identified, with one person excluded from the analysis. The first group, comprising 99 people (73.9%), presented with mild-to-moderate disease, which was most commonly characterized by lung (94.9%) and ENT manifestations (83.8%). Kidney involvement was less frequent (35.4%). Eosinophils were nearly as high as in typical EGPA.
The second group included 28 people (20.9%) with nonspecific body-wide, or systemic, symptoms (100%) and joint pain (92.9%). The third group included seven patients (5.2%) and had the most severe disease, with nonspecific systemic symptoms and severe kidney involvement (100% each) and frequent lung manifestations (85%).
PR3-ANCAs were more common in patients in groups 2 and 3 (78.6% and 71.4%, respectively) than in those from group 1 (54.5%).
The team then compared these groups with 656 people with typical EGPA and 229 typical GPA cases from other registry studies. They found that group 1 overlapped equally with both the typical EGPA (51.1%) and GPA (48.9%) groups, while groups 2 (89.3%) and 3 (100%) aligned predominantly with the typical GPA group.
By identifying three distinct clusters within overlapping forms, we provide novel insights into the [variability] of these conditions and their clinical implications.
Treatment to induce disease remission included glucocorticoids in nearly all participants across the three groups. Cyclophosphamide was used in all people from group 3, 60.7% of those in group 2, and 32.3% of group 1 patients. Rituximab, approved for GPA but not EGPA patients, was used in nearly 20% of participants in groups 1 and 2, but none in the third group.
Relapse rates were similar across the three groups, although relapse-free survival rates tended to be higher in people from groups 1 and 2 than in those from group 3. People in the third group had a significantly higher mortality rate (42.9% compared with 17.9% in group 2 and 9.2% in group 1).
Further statistical analysis showed that group 1 and the typical EGPA group had the best overall survival, while group 3 had the poorest. Relapse-free survival was highest in the typical EGPA group and lowest in group 3 and the typical GPA group.
Still, the team noted that the small number of patients in group 3 limits the statistical robustness of these results.
“By identifying three distinct clusters within overlapping forms, we provide novel insights into the [variability] of these conditions and their clinical implications,” the researchers wrote. “Future studies with larger [groups] and [follow-up] designs are essential to further define these overlapping forms, assess their long-term outcomes, and refine diagnostic and therapeutic approaches in AAV.”