IVIg therapy reduces relapses, eases disability in EGPA patients: Study
Treatment linked to 'good long-term control' of sensory, motor symptoms
Written by |
Intravenous immunoglobulin (IVIg) therapy can reduce relapses and lessen long-term disability in people with eosinophilic granulomatosis with polyangiitis (EGPA), a rare form of ANCA-associated vasculitis (AAV), a study from Italy has found.
At patients’ one-year follow-up after IVIg treatment, reductions in peripheral neuropathy — damage to nerves outside the brain and spinal cord — were reported among nearly 95% of those given the therapy. That compared with a reduction in such damage for slightly more than half of patients (52%) who did not receive this type of treatment.
“Our results indicate that add-on treatment with IVIg is associated with a good long-term control of sensory and/or motor symptoms, as well as with a lower risk of general and neurological relapses and better long-term disability outcomes,” the researchers wrote.
These data, the team added, “suggest a potential role of IVIg treatment in modifying [the] disease course as [an] add-on therapy to conventional treatments, especially in EGPA patients presenting [peripheral neuropathy] at disease onset.”
The study, “Effectiveness and safety of intravenous immunoglobulin for peripheral neuropathy in EGPA patients: a retrospective study,” was published in the Journal of Neurology.
Evaluating the effectiveness of IVIg therapy in EGPA patients
AAV is a group of autoimmune conditions that occurs when the body’s immune system erroneously attacks small blood vessels, causing inflammation and damage to them. These immune system attacks are typically triggered by self-reactive antibodies known as ANCAs that target neutrophils, a type of immune cell.
In EGPA, a type of AAV, patients develop granulomas, or clumps of immune cells known as eosinophils, in their blood vessels. These granulomas typically occur in the lungs and gastrointestinal tract.
About two-thirds of individuals with EGPA have peripheral neuropathy as an initial symptom, often manifesting as weakness, numbness, pain, and in some cases, partial paralysis. Peripheral neuropathy develops because blood vessels within nerves become inflamed, blocking blood flow to those nerves and damaging them.
“[Peripheral neuropathy] can significantly disrupt day-to-day functioning and quality of life and is associated with an increased risk of disability,” the researchers wrote.
Clinical guidelines recommend the use of high doses of corticosteroids along with immunosuppressive regimens to treat EGPA-related neuropathy. However, such treatment can have side effects, and neurological symptoms often persist.
Some researchers believe that intravenous immunoglobulin could be a potentially beneficial add-on therapy in EGPA patients with peripheral neuropathy. This retrospective, observational study now sought to evaluate the effectiveness of IVIg therapy for these patients.
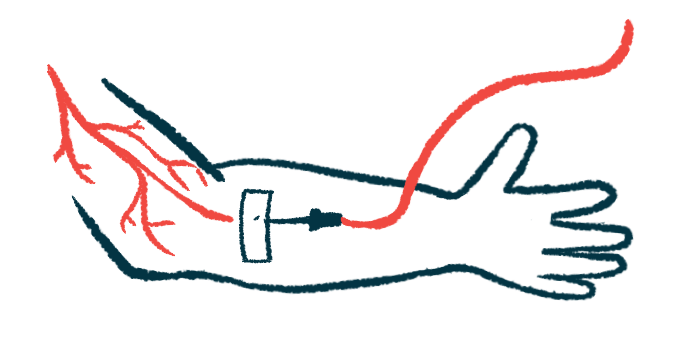
During IVIg treatment, patients receive an intravenous, or into-the-vein, infusion of different antibodies collected from the blood of healthy people. IVIg can neutralize harmful antibodies or immune responses in people with autoimmune conditions, like EGPA.
“Growing literature data indicate that the use of IVIg could be effective in inducing remission when disease activity persists despite standard therapy and that remission is maintained at long-term follow-up,” the researchers wrote.
Nearly 95% of IVIg-treated patients had a reduction in nerve damage
For their study, the team examined data from 39 patients with EGPA. All were treated with high doses of corticosteroids alone or associated with other traditional or biologic immunosuppressive drugs.
The patients were divided into two groups: an IVIg-treated group of 18, and a non-IVIg group of 21 individuals who were given only standard of care treatment.
The two groups were similar with the exception of ANCA positivity, which was significantly more common in the IVIg-treated group.
Overall, nearly two-thirds of the EGPA patients had multiple mononeuropathy, a condition marked by damage to several individual nerves in various areas of the body. More patients in the IVIg-treated group — more than 8 of every 10 — had multiple mononeuropathy, while almost half of those in the non-IVIg group had the condition.
The remaining patients had either polyneuropathy — neuropathy that affects several nerves, usually symmetrically — or mononeuropathy, in which neuropathy only affects one nerve.
At the last follow-up, 18 months after beginning treatment, 17 of 18 patients — 94.4% — in the IVIg-treated group experienced a reduction in peripheral neuropathy. The remaining one patient received a tapering dose of IVIg and worsened, experiencing the only relapse in the IVIg-treated group.
In the IVIg group, all the patients at last … follow-up presented a median [modified Rankin score of 1], which means achieving an almost complete independence in daily life thanks to a good recovery of weakness or pain in the extremities.
In the non-IVIg group, 11 of 20 patients had reduced neurological symptoms, while six patients remained stable and three saw their condition worsen.
In contrast to the one relapse seen in the IVIg-treated group, seven patients in the non-IVIg group experienced a relapse, six of whom had neurological symptoms.
The researchers also assessed long-term disability between the two groups using a measurement known as the modified Rankin score. On this seven-point scale, high scores mean more severe disability. Relative to the non-IVIg group, the IVIg-treated group had lower levels of long-term disability.
“In the IVIg group, all the patients at last … follow-up presented a median [modified Rankin score of 1], which means achieving an almost complete independence in daily life thanks to a good recovery of weakness or pain in the extremities,” the researchers wrote.
The team called for future placebo-controlled trials to confirm their findings.
“Further studies are necessary to assess the efficacy of IVIg add-on therapy in wider EGPA cohorts, as well as to define the optimal treatment duration and the safety of treatment discontinuation,” they concluded.






