Cardiac MRI can detect ANCA-associated vasculitis heart damage
Researchers: Conventional methods may not detect early involvement
Written by |
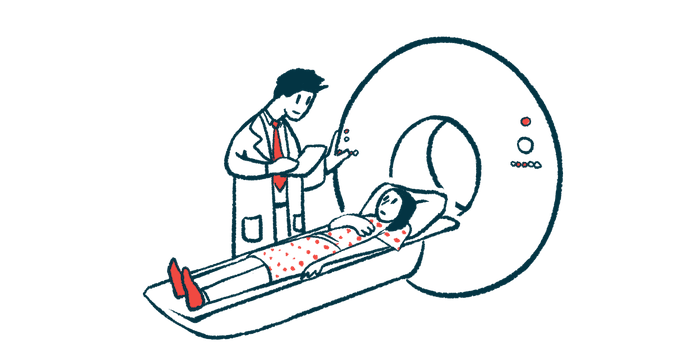
An imaging test that can make detailed pictures of the heart can detect scar tissue buildup in the heart muscle of adults with ANCA-associated vasculitis (AAV), even if they’re not having disease symptoms, a review study shows.
“Incorporating cMRI [cardiac MRI] into routine evaluations could improve the detection and management of cardiac involvement in patients with AAV,” wrote the researchers, who reviewed cMRI data from published studies of more than 1,000 patients. The study, “Cardiac Magnetic Resonance Imaging Findings in Patients With Antineutrophil Cytoplasmic Antibody–Associated Vasculitides: A Systematic Review,” was published in ACR Open Rheumatology.
AAV occurs when self-reactive antibodies prompt the immune system to launch an inflammatory attack on small blood vessels, causing damage to organs such as the kidneys and lungs. While it’s less common, the heart may also become involved.
“Cardiac involvement in AAV, although less common than [kidney] or pulmonary involvement, poses significant diagnostic challenges,” the researchers wrote, noting “conventional diagnostic tools such as electrocardiography (EKG) and echocardiography (TTE) may often fail to detect subtle [heart muscle] abnormalities.”
They warned that “this silent cardiac involvement can lead to underdiagnosis and delayed treatment.”
Cardiac MRI is typically superior to traditional imaging techniques at detecting heart muscle scarring, or fibrosis, inflammation, and other subtle changes. Here, researchers in the U.S. reviewed studies published up to March 2023 that reported on cardiac MRI measures in at least three adults diagnosed with AAV to better understand how well cardiac MRI can detect silent heart involvement in the disease.
Detecting heart damage tied to AAV
Thirty studies, covering 1,149 patients, were analyzed. The patients’ mean age was 52 and just over half were women. Regarding AAV types, more than 80% had eosinophilic granulomatosis with polyangiitis, while the remaining patients had either granulomatosis with polyangiitis or microscopic polyangiitis.
A key cardiac MRI measure is the left ventricular ejection fraction (LVEF), or the percentage of blood the heart’s left ventricle pushes out with each beat. A normal LVEF is usually 50% or higher.
The average LVEF in people with AAV was 55.6%, but more than a quarter (29%) had a LVEF below 50%, suggesting their left ventricle wasn’t pumping blood as well as it should.
Late gadolinium enhancement (LGE) is another valuable tool in a cardiac MRI. Presenting as a bright signal on the MRI, it’s a marker of myocardial, or heart muscle, fibrosis. Nearly half the patients had LGE, with scarring appearing most often on or around the inner heart lining (endocardial and sub-endocardial), followed by inside the heart muscle (intramyocardial) and beneath its outer layer (sub-epicardial).
Eight studies indicated “cMRI could detect subclinical myocardial involvement, even when EKG and TTE appeared normal,” the researchers wrote.
When comparing cMRI data between people in disease remission — meaning no or nearly no symptoms — or not, the team found that a significantly greater proportion of those in remission showed LGE, or myocardial fibrosis (55% vs. 47%). This difference was observed despite similar rates of abnormal electrocardiograms, which record the electrical activity of the heart, between the remission and non-remission groups (44% vs. 42%).
“The included studies consistently demonstrate a significant burden of subclinical cardiac involvement in AAV, particularly EGPA, as indicated by cMRI-detected myocardial fibrosis, even in patients who appear to be in clinical remission,” the researchers wrote.
“Clinicians should be aware that conventional diagnostic methods may not be sufficient to detect early cardiac involvement,” they concluded. “Incorporating cMRI into the standard evaluation of patients with AAV, even those in clinical remission or without cardiac symptoms, may facilitate early detection and intervention, potentially improving long-term cardiovascular outcomes.”