ANCAs may hold unique role in vessel inflammation with EGPA
Relapses outside respiratory system seen only in patients positive for ANCAs
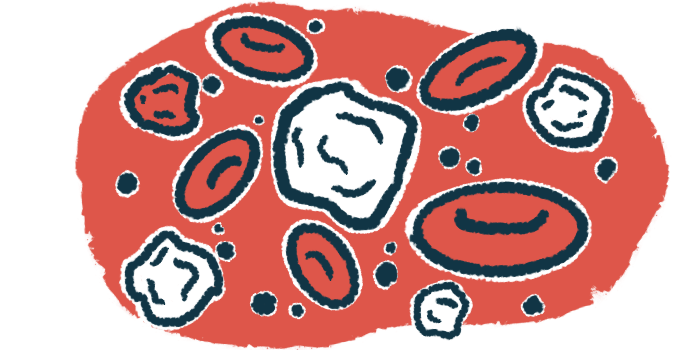
Self-reactive anti-neutrophil cytoplasmic antibodies, or ANCAs, may play a unique role in driving blood vessel inflammation in people with eosinophilic granulomatosis with polyangiitis (EGPA), the rarest form of ANCA-associated vasculitis (AAV).
That’s according to a small study, which found that disease relapses outside the respiratory system occurred only in EGPA patients positive for ANCAs, while levels of eosinophils — the immune cells that characterize and are thought to drive EGPA — remained normal.
According to the researchers, EGPA’s underlying mechanisms may involve two distinct factors: eosinophils, which are sensitive to eosinophil-targeted therapy, and ANCAs, which are responsive to immunosuppressive treatments. If proven with further studies, this finding could have important implications for how EGPA is managed.
The study, “ANCA-negative EGPA: only eosinophils without vasculitis? Insights from anti-T2 biologics,” was published in Frontiers in Immunology.
Whether ANCAs are disease driving in EGPA is still under debate
EGPA is the rarest type of AAV, a group of autoimmune disorders characterized by inflammation in small blood vessels, eventually damaging tissues and organs.
This rare form is characterized by the accumulation of immune eosinophils into masses in small blood vessels. Patients have a wide array of disease symptoms, most commonly affecting the respiratory system.
Only about 1 in 3 EGPA patients are positive for ANCAs, the self-targeting antibodies that cause most AAV cases. Whether or not ANCAs are truly disease driving in EGPA is still a matter a debate, “while the role of eosinophils is well established,” the researchers wrote.
In recent years, Nucala (mepolizumab) has been approved as an add-on to immunosuppressive treatment for certain EGPA patients in the U.S. and in Europe. It works to reduce eosinophil levels by blocking a signaling molecule called IL-5 that promotes their growth, maturation, and survival.
Scientists in Italy looked into the clinical outcomes of 13 people with EGPA who were treated at their clinic between 2018 and 2023. At diagnosis, all but three patients had respiratory and extra-respiratory manifestations, or those affecting organs and tissues outside the respiratory system. Five of the 13 patients were positive for ANCAs.
All initially were given high-dose corticosteroids, often with other immunosuppressive treatments, which was the standard-of-care for EGPA prior to Nucala’s availability. This resulted in complete clinical remission, eosinophil normalization, and the absence of ANCAs in the five previously positive patients.
In the meantime, Nucala and benralizumab — a therapy sold as Fasenra that works in a similar way and has also shown promise in EGPA — were approved to treat severe eosinophilic asthma, which affected all of these EGPA patients.
EGPA patients who relapsed with treatment were ANCA positive at diagnosis
All patients then were given Nucala or benralizumab. Based on response, some switched from one therapy to the other or to dupilumab (sold as Dupixent), which also acts to reduce eosinophil activation.
These eosinophil-suppressing medications helped maintain normal eosinophil levels and symptom control, including of asthma. All but one patient discontinued immunosuppressive treatment due to lack of efficacy, remission of extra-respiratory manifestations, or side effects.
During eosinophil-targeting treatment, five patients had extra-respiratory relapses, manifesting for all as pain in muscles and joints. Other reported symptoms included fever and skin abnormalities.
Notably, these five people were those positive for ANCAs at diagnosis. Based on updated diagnostic criteria published in 2022, they also were the only ones with definitive vasculitis (blood vessel inflammation) when diagnosed.
While they no longer showed ANCAs after initial immunosuppressive treatment rounds, most showed an increase in these self-reactive antibodies during the relapses. However, their eosinophil levels generally stayed within normal ranges.
Taking these findings collectively, the researchers proposed that ANCAs may play a unique role in EGPA, driving disease in a manner that’s separate and distinct from the actions of eosinophils.
“In patients undergoing [Nucala]/Benralizumab, eosinophils were within the normal range during extrarespiratory relapses. Therefore, we hypothesized that extrarespiratory relapses might be due to the raised [levels of ANCAs],” the scientists wrote.
“These observations may raise the question whether EGPA vasculitis exists only in [ANCA-positive] patients, and whether [ANCA-negative] disease is only [eosinophil-related] inflammation without vasculitis,” they added.
If this is the case, then the ANCA-negative patients in this study might be said not to truly have EGPA, but instead to have other inflammatory disorders driven by excessive eosinophils.
The researchers noted only a few reports exist of ANCA-negative EGPA patients experiencing organ vasculitis. They speculated that these cases might be false negatives or caused by other conditions that look like vasculitis but aren’t.
Due to the small number of patients in this study, more work is needed to verify whether this hypothesis will hold up, the scientists noted. But “if confirmed by larger studies, these observations may have important therapeutic implications, possibly leading to a [mechanism-based] therapy of EGPA,” they concluded.