AAV Rare in COPD Patients With AAT Deficiency, Study Finds
Written by |
Low levels of the protein alpha-1-antitrypsin (AAT) do not appear to be enough to increase the risk of ANCA-associated vasculitis (AAV) in people with chronic obstructive pulmonary disease (COPD) — despite prior associations of AAT deficiency with AAV — according to a new study.
The study, “Prevalence of Anti-Neutrophil Cytoplasmic Antibodies and Associated Vasculitis in COPD Associated With Alpha-1 Antitrypsin Deficiency: An Ancillary Study to a Prospective Study on 180 French Patients,” was published in the journal Chest.
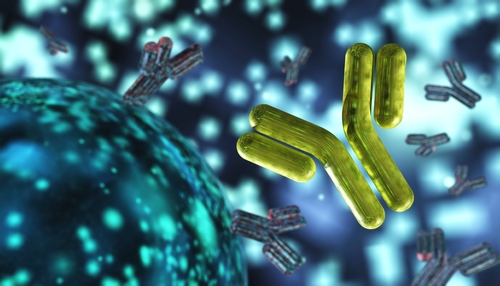
AAV is a group of autoimmune diseases characterized by inflammation in and damage to small blood vessels. In AAV, autoantibodies called ANCAs target a type of immune cells known as neutrophils, which are essential for fighting infection.
These autoantibodies are generally directed at two proteins — proteinase 3 (PR3) and myeloperoxidase (MPO) — found in the neutrophils. When the ANCAs bind these proteins, the neutrophils release toxic substances that are harmful to the blood vessels.
The AAT protein is known to affect neutrophil function and the interaction of ANCAs with the PR3 protein. A deficiency in this protein, caused by mutations in the SERPINA1 gene, has been linked to autoimmune disorders such as AAV.
People with COPD, a progressive lung disease that causes breathing difficulties, have been found to have an AAT deficiency. Two of the most common conditions associated with COPD are chronic bronchitis — inflammation of the lining of the airways that makes it harder to breathe — and emphysema, which is damage to the air sacs in the lungs that causes shortness of breath.
Here, AAT controls the activity of another protein, called neutrophil elastase, which is released by neutrophils to digest bacteria. In the absence of AAT, excess neutrophil elastase activity causes damage in the lungs, leading to COPD.
Given the connection between AAT deficiency in AAV and people with COPD, researchers based at the Caen University Hospital in France wondered if COPD patients with an AAT deficiency would be predisposed to ANCA autoantibody production or AAV.
To find out, patients were recruited from the CONEDAT clinical trial (NCT00700934), being conducted in Paris. The goal of that large, ongoing study is to describe the natural history of people with AAT deficiency-associated emphysema and to identify factors related to prognosis.
The CONEDAT group included French patients, ages 18 and older, whose clinical data were collected every six months over five years. Among the 416 individuals included in CONEDAT, blood samples were available for 185 patients. Five people were excluded due to a lack of genetic information.
Blood serum from the participants was tested for the presence of anti-PR3 and anti-MPO autoantibodies. While clinical data suggestive of AAV also were examined, none of the patients had been diagnosed with AAV.
The serum analysis also found that none of the patients tested positive for anti-MPO antibodies; one patient had anti-PR3 antibodies. However, based on the medical history, which included a one-year follow-up, this patient had no signs of AAV.
The prevalence of AAV in this group of patients was 0%, based on these results. According to the investigators, that “is not different from the estimated prevalence in the general population (0.006%).”
“To conclude, although AAT deficiency is statistically overrepresented among patients with ANCA-associated vasculitis and might be involved in its pathophysiology, the mere presence of AAT deficiency does not seem to expose these patients to an increased risk of ANCA-associated vasculitis,” the researchers wrote.
Because of the low prevalence, “systematic screening appears not to be appropriate,” they added.