2 AAV types better suggest clinical features, outcomes in study
Differences among MPA, GPA, and other forms noted by researchers
Written by |
Having microscopic polyangiitis (MPA) or granulomatosis with polyangiitis (GPA) — the two most common types of ANCA-associated vasculitis (AAV) — better determines patients’ clinical features and outcomes than the type of AAV-driving, self-reactive antibodies they have.
That’s according to a study in Spain that showed that GPA was an independent risk factor of disease relapse and was more often linked to symptoms in the ears, nose, and throat (ENT), as well as eye problems. It also indicated a better survival prognosis than MPA.
Having antibodies against the proteinase 3 (PR3) enzyme, one of the two most common types of AAV-driving antibodies and one commonly associated with GPA, were also more commonly associated with ENT and eye symptoms, but not to other outcomes.
The study, “Significance of clinical-immunological patterns and diagnostic yield of biopsies in microscopic polyangiitis and granulomatosis with polyangiitis,” was published in the Journal of Internal Medicine.
ANCA types are an independent feature of AAV types. In AAV, abnormal immune responses ultimately lead to damaging inflammation in small blood vessels. These immune attacks are driven mostly by self-reactive antibodies, called ANCAs, that most commonly target one of two enzymes: myeloperoxidase (MPO) and PR3.
MPA and GPA are associated with somewhat distinct symptoms. In addition, MPA is strongly linked to anti-MPO ANCAs; GPA is often associated with anti-PR3 ANCAs.
“Although the role of ANCA type in disease extent, severity, relapses, and mortality has been explored with controversial results, patients with MPA and MPO-ANCA have been reported as having worse … survival in some large European and Northern American series, and GPA and PR3-AAV have been repeatedly associated with higher relapse rates,” the researchers wrote.
The study and its data
To assess the impact of AAV and ANCA types on clinical presentation and prognosis, a team of researchers in Spain and Portugal looked back at data from 152 people with MPA or GPA collected from 2000 to 2021 at a single Spanish reference center.
More than half (57.9%) were women, and most (86.8%) were Caucasian. A total of 77 patients had MPA, whereas the remaining 75 had GPA. Nearly two-thirds (65.1%) had anti-MPO ANCAs, and 23% had ANCAs against PR3.
Most people with MPA (96.1%) tested positive for ANCAs against MPO. In contrast, many people with GPA tested positive for ANCAs either against PR3 (44%) or MPO (33.3%).
Nearly a quarter of GPA patients (22.7%) tested negative for ANCAs or had atypical ANCAs against other proteins, while that was the case of only one MPA patient (1.3%).
Compared with GPA patients, those with MPA had significantly shorter disease duration and were significantly more likely to experience weight loss, muscle pain, kidney involvement, and interstitial lung disease (ILD), which occurs when the airways become scarred, making it difficult to breathe.
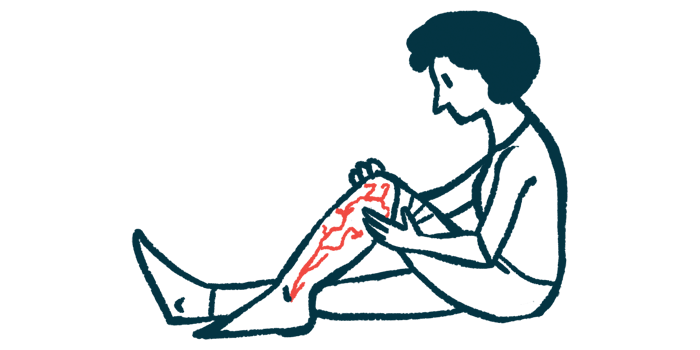
They were also significantly more likely to have purpura, a skin condition marked by small reddish-purple spots caused by burst small blood vessels and the involvement of peripheral nerves, which are bundles of nerve fibers outside the brain and spinal cord.
People with GPA presented significantly more often with ENT and eye symptoms, lung nodules, and skin problems other than purpura. GPA patients also had significantly more relapses, but better survival rates than MPA patients.
Patients with anti-MPO ANCAs presented with muscle pain, ILD, and uveitis (a type of eye inflammation) significantly more frequently than those with anti-PR3 ANCAs. In turn, anti-PR3 ANCAs were significantly associated with a greater frequency of lung nodules, as well as ENT and eye involvement.
Further statistical analyses showed that having a GPA diagnosis “was the only independent risk factor for relapse,” the researchers wrote. Being 68 years or older at diagnosis and peripheral nerve involvement were each significantly linked to an increased risk of death.
Among GPA patients, those with anti-PR3 ANCAs were more often men and were significantly more likely to have lung bleeding than those with anti-MPO ANCAs. No other significant differences were detected for clinical manifestations, relapse, or survival in terms of ANCAs against PR3 versus MPO.
These findings highlighted that AAV types were better than ANCA types at determining clinical features and outcomes.
“Awareness of risk factors for relapse and mortality are important to guide proper therapeutic strategies in AAV patients,” the researchers wrote.
A total of 152 AAV patients had undergone a mean of 1.5 biopsies in at least one affected tissue, and more than a third (37.7%) had had two or more because of a previous biopsy showing negative or inconclusive results. A biopsy is a procedure to remove a piece of tissue from the body so that it can be sent for testing.
Vasculitis, or blood vessel inflammation, was detected in 97.3% of people with MPA and 61.8% of those with GPA.
Additional analyses “demonstrated that the performance of more than one biopsy in different territories (when a previous procedure resulted in negative or inconclusive) offers a higher diagnostic yield for vasculitis than that provided by isolated biopsies,” the team wrote.
“Biopsies of different affected territories should be pursued in difficult-to-diagnose patients based on their significant diagnostic yield,” they concluded.