Elevated Microparticle Levels in AAV Patients Mark Higher Risk of Blood Clots, Study Suggests
People with anti‑neutrophil cytoplasmic antibody (ANCA)‑associated vasculitis (AAV) who have high levels of cellular microparticles in their blood may be at higher risk for venous thromboembolism (VTE), a life-threatening blood-clotting condition, a recent study suggests.
A 10% increase in microparticles represented a 40% increased risk of VTE, the researchers said.
The study, “Elevated Microparticle Tissue Factor Activity Differentiates Patients With Venous Thromboembolism in Anti-neutrophil Cytoplasmic Autoantibody Vasculitis,” was published in the journal KI Reports.
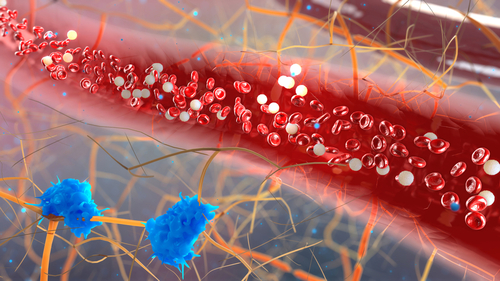
AAV is a term for a group of autoimmune disorders causing inflammation and swelling of small blood vessels.
About 8% to 16% of people with the condition are at risk for VTE in which blood clots form, usually in the deep veins of the leg, groin, or arm. These clots can break off and travel to the lungs, blocking blood flow, a condition called a pulmonary embolism.
Despite this high risk, little is known about the mechanisms that drive VTE in AAV, and current biomarkers of VTE — molecules in the blood used to track disease — are not entirely specific.
Studies have identified antibodies that target plasminogen (Plg) — a protein involved in blood clot formation — as a possible contributor to the development of VTE, as antibody binding would delay the removal of blood clots.
Also implicated in VTE are microparticles (MPs), which are cell fragments shed by cells that circulate in the blood of patients with various diseases. MPs are elevated in AAV patients during active disease, and cells treated with ANCAs and MPs lead to increased blood clot formation.
A team of investigators at the University of North Carolina designed a study to follow a group of AAV patients to determine if elevated levels of anti-Plg antibodies or MPs could identify patients at risk for VTE.
A total of 41 AAV patients were recruited, along with 70 healthy people used as controls. Of the patients, 29 were negative for VTE, while 12 were positive. Eleven patients developed VTE during the study.
Blood samples were collected and analyzed, and clinical assessments were conducted during active disease, which is when VTEs tend to occur. The median follow-up time for VTE-positive patients was 21.5 months, and 24.9 months for those without VTE.
The blood tests revealed that anti-Plg levels were significantly higher in patients with active AAV than in those without active disease or healthy controls.
While higher anti-Plg levels were detected in those with active disease compared with healthy controls, patients who experienced VTE had levels of anti-Plg antibodies similar to those without VTE.
High anti-Plg during remission implied enhanced blood clotting was still active, the researchers said. This “suggests that some patients with ANCA vasculitis and detectable anti-Plg, even within a normal reference range, may be at risk for VTE during remission,” they wrote.
MP levels were significantly higher in patients who experience VTE than in those who did not. Notably, the MP levels in VTE-negative patients were the same as healthy controls.
An analysis before VTE development found that MP levels were closely associated with VTE regardless of whether patients had active disease.
Additional blood tests showed that low levels of serum albumin — a protein marker for liver and kidney disease — was associated with a fourfold increased risk of VTE.
“Our study identified elevated MPTFa [MP], increased anti-Plg during remission, and hypoalbuminemia as novel biomarkers associated with VTE in patients with ANCA vasculitis,” the authors said. “These hypothesis-generating studies contribute to our understanding of the mechanisms of VTE and form a foundation for future studies.”





