Certain immunosuppressants linked to better survival after brain bleeds
Glucocorticoids, in contrast, tied to worse outcomes in AAV in review
Written by |
Treatment with the immunosuppressants cyclophosphamide, azathioprine, or rituximab after ANCA-associated vasculitis (AAV) patients have experienced a brain bleed, or intracranial hemorrhage, is linked to better survival, according to a review of previously reported cases.
“In our pooled analysis, we found that initiating [immunosuppressant] treatment after [brain bleeds] … was significantly associated with improved survival,” the team wrote.
In contrast, the use prior to a brain bleed of glucocorticoids, a type of anti-inflammatory and immunosuppressive medication, was associated with worse survival, the data showed. That finding highlights “the importance of glucocorticoid-sparing strategies in managing [brain and spinal cord] involvement in AAV,” the researchers wrote.
The review study, “Risk of intracranial hemorrhage in anti-neutrophil cytoplasmic antibody-associated vasculitis treated with glucocorticoids: a systematic review of case reports,” was published in the journal Rheumatology International.
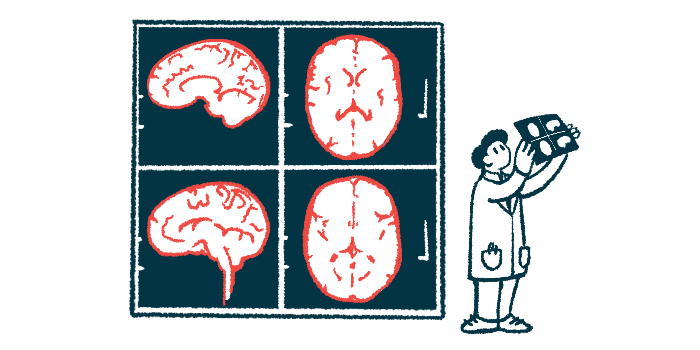
AAV occurs when the immune system mistakenly attacks small blood vessels, causing inflammation and damage to organs. Although rare, AAV can affect the central nervous system, known as the CNS, which comprises the brain and spinal cord. Little is known about this complication, however.
“Rare cases of CNS involvement, particularly intracerebral hemorrhage (ICH), in AAV have been reported, but risk factors remain poorly defined,” the researchers wrote.
Investigating treatments and outcomes of brain bleeds in AAV
To better understand the risk factors, treatment options, and outcomes of brain bleeds in people with AAV, a team of researchers in the U.S. conducted a review of medical literature. Specifically, the team looked for reports of AAV complicated by intracranial hemorrhage, published through October 2024.
A total of 46 studies, describing 47 patients, were included in the final analysis. The patients had an average age of 49.4, and slightly more than half were men.
Regarding AAV types, 48.9% of patients had eosinophilic granulomatosis with polyangiitis, 29.8% had granulomatosis with polyangiitis, and 14.9% had microscopic polyangiitis. Most of them (85.1%) were diagnosed with AAV only after experiencing a brain bleed.
The most frequent type of brain bleed was intraparenchymal hemorrhage (55.3%), which is bleeding within brain tissues, followed by subarachnoid hemorrhage (29.8%), or bleeding in the space below one of the thin layers that cover the brain.
Less frequent types of intracranial hemorrhage included intraventricular hemorrhage (8.5%), or bleeding into the brain’s fluid-filled spaces, and subdural hemorrhage (6.4%), which is bleeding between the brain and its outer covering.
Cyclophosphamide, azathioprine, or rituximab linked to better survival
While slightly more than half of patients (57.4%) had not received any immunosuppressive treatment for AAV — meaning cyclophosphamide, azathioprine, rituximab, or mycophenolate mofetil — before a brain bleed, the same proportion experienced this complication after starting treatment with glucocorticoids.
Two-thirds of patients (66%) survived the episode of AAV-related brain bleed. Statistical analyses showed that those who died were significantly older than those who survived (58 vs. 45 years), and were significantly more likely to have been on glucocorticoids prior to the brain bleed (93.8% vs. 40%).
Glucocorticoids have long been associated with decreased [blood vessel] structural integrity, which may contribute to an increased risk of bleeding. … A gradual shift toward low-dose glucocorticoid regimens, particularly in high-risk or frail patients, is now recommended.
Further analyses demonstrated that each additional year of age increased the odds of death by 6.8%, while glucocorticoid treatment prior to a brain bleed was linked to 25 times higher odds.
“Glucocorticoids have long been associated with decreased [blood vessel] structural integrity, which may contribute to an increased risk of bleeding,” the researchers wrote. “A gradual shift toward low-dose glucocorticoid regimens, particularly in high-risk or frail patients, is now recommended.”
When started after the brain bleed event, use of the immunosuppressants cyclophosphamide, azathioprine, or rituximab was significantly linked to better survival.
However, almost all patients who died (93.8%) never received any treatment after experiencing this complication. Some were transitioned to comfort care before any potential immunosuppressive treatment.
“Treatment after an episode of ICH was linked to improved survival,” the researchers wrote.
Still, the team called for additional studies “to improve patient outcomes in AAV.”
“Further research with larger [groups of patients] is necessary to validate these findings and refine treatment strategies, including exploring glucocorticoid-sparing options,” the researchers wrote.