Complement System Overactive in AAV Patients With Active Disease, Study Finds
The complement system, a part of the immune system, is overactive in people with active ANCA-associated vasculitis (AAV), but achieving remission appears to lower most of its components to normal levels, a study reports.
The study, “The alternative complement pathway in ANCA‐associated vasculitis: further evidence and a meta‐analysis,” was published in Clinical & Experimental Immunology.
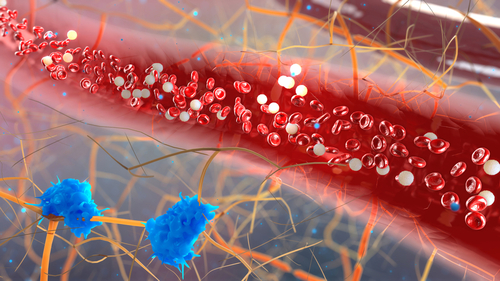
The complement system consists of a group of proteins that are normally present in the blood in an inactive state. However, in response to an inflammatory stimulus (for instance, an infectious bacteria), a chain reaction converts many of the proteins into active states. Then, the proteins can help drive an immune response by promoting inflammation and helping to kill infectious invaders.
This system may also play a role in autoimmune diseases — conditions where the immune system attacks the body’s healthy tissue, such as AAV. Some previous studies have implicated complement activation in AAV, but these studies typically included relatively few people, limiting the strength of the findings.
In this study, researchers at the Sechenov First Moscow State Medical University, in Russia, measured levels of activated complement proteins in the blood of 59 people with AAV (62.7% female, average age 52.5 years), including 41 with granulomatosis with polyangiitis and 18 with microscopic polyangiitis. For comparison, levels were also measured in 36 people without AAV (75% female, average age 55.7 years).
Compared with controls, people with active AAV had significantly higher levels of activated complement components, including complement 5a (C5a), complement 3a (C3a), membrane attack complex (MAC), and factor B.
In 28 patients, complement assessments were also collected during remission. When remission was achieved, C5a, C3a, and factor B levels lowered significantly compared with their levels during active disease. Only MAC and properdin did not change following remission induction therapy.
Nevertheless, the researchers noted a lot of person-to-person variability in levels, regardless of remission status.
“Signs of complement activation were found only in a proportion of patients with active AAV, whereas achievement of clinical remission following immunosuppressive therapy did not always lead to normalization of various complement component levels,” they wrote. “Therefore, we cannot conclude that any plasma complement component alone may be useful as a biomarker of the disease activity or a guide for treatment decisions.”
There were no significant differences noted in levels of complement proteins based on ANCA type, AAV type, treatment, or disease severity. Additionally, complement protein levels were not significantly associated with clinical or laboratory markers (e.g., creatinine levels, which are indicative of kidney health).
The researchers then combined their data with data from four previously published studies that also assessed the role of the complement system in AAV. The number of people analyzed varied among the individual complement proteins; the largest analysis was for C3a, which included 223 people with active AAV, 192 with AAV in remission, and 124 without AAV.
This meta-analysis indicated that levels of C5a and MAC were significantly higher in people with active AAV than in those in remission or those without AAV. Other components (e.g., C3a and factor B) followed similar trends, but the differences did not reach statistical significance.
Of note, in the chain reaction of complement activation, C5a and MAC are activated toward the end. As such, elevated levels of these markers could be generally reflective of increased activity in the system as a whole.
“In our and previous studies, the terminal pathway components levels, that is C5a and MAC, were elevated in patients with active AAV compared to healthy controls. This finding indicates that complement activation occurs in the course of systemic vasculitis,” the researchers wrote.
However, the researchers again noted the considerable person-to-person variability, and that “analysis of both complement components [C5a and MAC] alone does not allow for distinction between active disease and remission.”
The largest limitation of this study is its small sample size, particularly in evaluating remission compared with active disease.
“However, our findings are in accordance with previous studies and were reinforced by the meta-analysis of all available data on activation of the complement system in AAV,” the investigators concluded.






