ANCA-Associated Vasculitis can Result in Appendicitis Without Other Systemic Symptoms, Case Report Shows
Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis can result in inflammation of the appendix — commonly known as appendicitis — without any additional systemic symptoms, researchers report for the first time.
The finding highlights the diverse effects of this autoimmune disorder and the importance of careful patient evaluation for adequate diagnosis and care.
Researchers from the Royal North Shore Hospital in Sydney, Australia, wrote about the case study in a letter, titled “ANCA-associated vasculitis of the appendix,” that was published in the journal Rheumatology Advances in Practice.
In their report, a 27-year-old female patient was referred to hospital after four days of right upper quadrant and flank pain, and high-grade fever. These symptoms were preceded by upper respiratory tract symptoms, including coughing and sneezing, as well as lack of energy, general discomfort, and weight loss in the prior six months. She also reported experiencing similar episodes of abdominal pain that lasted for one day in the previous two months.
She was first treated for inflammation of the right kidney. In an initial evaluation, she was found to have high levels of white and red blood cells in the urine, which are hallmarks of kidney infection by bacteria or other microorganisms. However, the treatment failed to reduce or manage her symptoms, and she started to experience worse abdominal pain.
Images from an abdominal computerized tomography (CT) scan suggested that she had either a kidney inflammation due to infection or an obstruction of the blood supply to the kidney.
She underwent laparoscopic surgery, which allows doctors to evaluate the inside of the abdominal cavity without large incisions. During this procedure, it was confirmed that her right kidney was experiencing reduced blood supply.
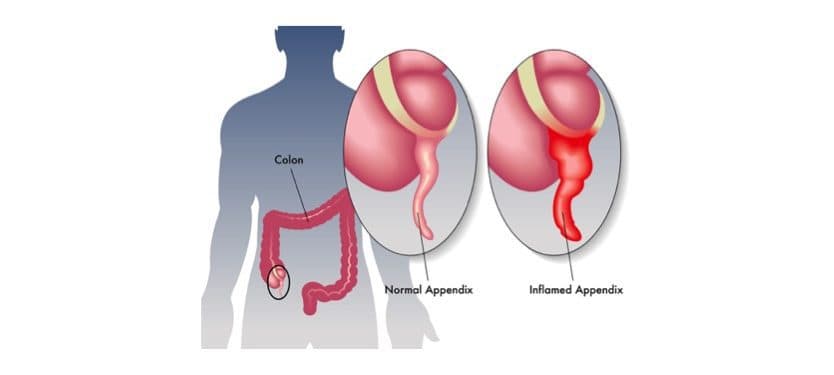
Surgeons also decided to remove her appendix, which was discolored, as a preventive measure to exclude appendicitis as a possible cause of her abdominal pain. Still, evaluation of the appendix did not reveal any tissue abnormalities.
Blood laboratory analysis showed that she was positive for both cANCA and anti-PR3 antibodies, and had high levels of inflammatory biomarkers. She was found to be positive for lupus anticoagulant antibodies.
Although initial urine analyses performed before surgery showed high levels of red blood cells, subsequent evaluations were all within normal ranges.
Additional CT evaluation of her kidney confirmed that the main renal arteries were blocked, and that she had mild inflammation. To help resolve this blockage, she started treatment with enoxaparin (sold by Sanofi as Lovenox).
Since she was also positive for autoantibodies often linked to ANCA-associated vasculitis (AAV), the researchers decided to take another look at her appendix. The new examination revealed that immune cells had infiltrated the appendix lining tissue, causing tissue damage to the vessel walls and cell overgrowth. These findings led to the diagnosis of small-vessel vasculitis of the appendix.
Her clinical condition remained stable during followup, with anti-PR3 antibody levels approximately five times higher than the upper normal limit. However, she did not experienced any antibody-related systemic symptoms in need of immunosuppressive therapy.
Contrary to what happened to the patient, “vasculitis involving the gastrointestinal tract is most commonly associated with medium-vessel vasculitis (…) and usually occurs as part of the systemic vasculitic process,” the researchers reported.
“To our knowledge, our case is the only published case of AAV with isolated involvement of the appendix,” providing for the first time evidence that “AAV can cause appendicitis in the absence of systemic manifestations,” they said.
“These patients need to be followed closely to monitor serological positivity [presence of abnormal antibodies] and for the development of systemic features requiring immunosuppression [medications that block the overactive immune system],” the authors said.






