Other conditions, processes may mimic CNS involvement in AAV
Researchers in Turkey assessed potential mimickers' prevalence in disease
Written by |
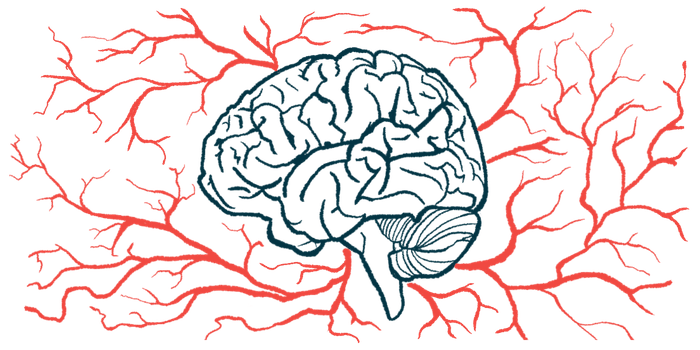
In ANCA-associated vasculitis (AAV), the involvement of the central nervous system (CNS), that is, the brain and spinal cord, is uncommon, but other factors may mimic CNS involvement, a study reports.
These so-called mimickers can include AAV disease processes not related to the CNS, other conditions, and drug-related adverse events.
“The extent to which these mimickers contribute to symptoms suggesting CNS involvement was not well studied,” wrote the researchers, who found mimickers accounted for nearly three-quarters of AAV patients with neurologic symptoms. Less than 2% of the 430 people with AAV evaluated received a definitive diagnosis of CNS involvement. The study, “Central nervous system involvement and mimickers in ANCA associated vasculitis,” was published in the Journal of Neurology.
In AAV, abnormal immune processes result in inflammation and damage to small blood vessels, part of the vascular system. Symptoms can vary depending on the AAV type and where the damage occurs. The kidneys, respiratory system, and peripheral nervous system (PNS), that is, the nerves outside the CNS, are often affected in AAV. CNS involvement, however, “seems to be a rare manifestation of AAV, irrespective of the type of AAV,” the researchers wrote.
Studies have reported CNS involvement in about 5% to 15% of people with AAV. The symptoms associated with it may include headaches and a potentially increased risk of stroke.
Treatment for AAV often includes glucocorticoids, which can help reduce inflammation, and immunosuppressive therapies. Evidence of CNS involvement may prompt physicians to choose a more aggressive treatment course. Although this may increase the chance of remission, it can also increase the risk of side effects, such as infection.
Diagnoses of CNS involvement
Symptoms consistent with CNS involvement don’t guarantee actual CNS involvement, however, which complicates this kind of treatment decision. To assess potential mimickers and their prevalence in AAV, researchers in Turkey examined the medical records of 430 people with AAV. Of these, 61 (14%) exhibited potential signs or symptoms of neurological involvement that required a neurological examination. The mean age of this group was 51.6. About two-thirds had granulomatosis with polyangiitis and the rest were split between other AAV types. All had active disease when their neurological symptoms occurred, and 34% had PNS involvement.
Seven people — 1.6% of all the participants and 11.5% of the group with neurological involvement — ultimately received diagnoses of CNS involvement. Among these, neurological symptoms appeared an average of 10 months after their AAV diagnosis and were the initial disease manifestation in two patients. All had additional disease manifestations in other body systems.
“These results may suggest that CNS involvement is mostly observed in the early years of AAV and it is accompanied by another active organ involvement in all patients,” the researchers wrote.
The most common CNS symptoms were headache, muscle weakness, seizures, and numbness, with each appearing in three of the seven participants. Three patients also had PNS involvement. Two participants’ neurological symptoms were considered related to stroke, a vascular event that’s more common among people with AAV than in the general population.
“However, it is difficult to conclude whether these manifestations are part of [blood vessel] involvement or due to [bodywide] inflammation,” the researchers wrote.
The remaining five patients had AAV involvement in brain membranes, blood clots in the brain, or increased blood pressure inside the skull. All seven patients with CNS involvement received treatment with immunosuppressive agents and all but one recovered, generally not without complications.
Frequency of mimickers in AAV
In nearly half the group with neurological symptoms, a neurologic examination showed that non-CNS manifestations of AAV were causing the symptoms. The most common cause was PNS involvement, followed by involvement of the upper respiratory tract and the eyes or surrounding tissues. All these participants were given immunosuppressive treatment and all but three recovered without complications.
Reactions to medications or separate conditions, including cardiovascular events and infections, explained about a quarter of the cases with neurological symptoms. This left about 15% of participants without a definitive diagnosis for their neurological symptoms.
The results suggest mimickers account for more cases of neurological symptoms in AAV than CNS involvement.
The proportion of total participants who had neurological symptoms was similar to that from previous studies. More restrictive criteria revealed less than 2% of the group had CNS involvement, however.
“Before intensifying immunosuppressive treatment in patients presenting with CNS symptoms, mimickers should be ruled out to minimize the potential harm associated with immunosuppression,” wrote the researchers, who noted the most consistent way to establish CNS involvement is by examining samples of brain tissue, which weren’t available in this study. The researchers therefore made some subjective judgements about what to consider CNS involvement. Future studies could use biological markers to more objectively determine the relative frequency of CNS involvement and mimickers.