Mitochondrial DNA May Serve as Urinary Biomarker of Kidney Damage, Chinese Study Suggests
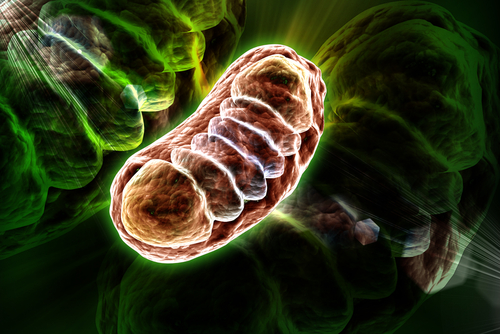
Mitochondrial DNA (mtDNA) — DNA specific to mitochondria, the cell’s powerhouses — may be used as a urinary biomarker of kidney damage in people with ANCA-associated vasculitis (AAV), according to a Chinese study.
The study, “Urinary mitochondrial DNA is a useful biomarker for assessing kidney injury of antineutrophil cytoplasmic antibody-associated vasculitis,” was published in the journal Clinica Chimica Acta.
AAV is a chronic autoimmune disease associated with the inflammation and destruction of small blood vessels. Most people with AAV develop kidney disease and are at risk of end-stage renal disease (ESRD), which occurs when the kidneys no longer work efficiently.
While kidney biopsy is the gold standard for diagnosing kidney involvement in people with AAV, not all patients have the chance to undergo the procedure. Thus, there is an unmet need for new biomarkers for kidney damage in AAV patients.
Recent studies have shown that the detection of mtDNA in the urine — due to mitochondrial damage — may be used as a biomarker of kidney impairment. Increased levels of urinary mtDNA also showed associations with disease severity and progression, the rate of kidney function decline, and the likelihood of developing ERSD in several kidney diseases.
However, no study to date has investigated the potential association between urinary mitochondrial DNA levels and kidney damage in AAV patients.
Now, researchers at Tianjin Medical University General Hospital, in China, evaluated whether urinary mtDNA could be used as a biomarker of kidney damage in AAV.
To do so, they analyzed the data of 39 people — 22 men and 17 women — with MPO-positive AAV and biopsy-confirmed kidney damage, and 10 age-matched healthy volunteers. Among the patients with AAV and kidney damage, 33 (85%) had kidney dysfunction and 13 needed dialysis at disease onset.
Biopsies usually are classified into four classes: focal, crescentic, sclerotic, and mixed. This depends on how poor the kidney function is, and on the health of the glomeruli, the kidney’s filtration units. A total of 14 patients were classified as mixed class, with 13 as focal class, and 12 as crescentic class.
The results showed that urinary mtDNA levels were significantly higher in the AAV patients than in the healthy people, and that the individuals needing dialysis at disease onset had the highest levels.
Further analyses highlighted that higher levels of urinary mtDNA were significantly associated with greater levels of urinary neutrophil gelatinase-associated lipocalin (NGAL) — an early marker of kidney damage — and with poorer kidney function, as assessed through the estimated glomerular filtration rate. These higher levels also were associated with other kidney damage-associated features, including infiltration of neutrophils — the most abundant white blood cell in the circulation — in the kidney.
These data suggest that urinary mtDNA levels, potentially in combination with urinary NGAL, could be used as a biomarker of kidney damage and dysfunction, as well as of its severity, in people with AAV.
The team also noted that patients with kidney damage classified as crescentic had significantly higher urinary mtDNA levels than patients in the other two classes, suggesting that this class is associated with more active kidney damage.
Moreover, patients who recovered their kidney function after three months of dialysis had higher levels of urinary mitochondrial DNA than those who remained dialysis-dependent. This suggests that higher levels of mtDNA may predict a greater therapeutic benefit from dialysis.
The researchers noted, however, that since all patients in their study were MPO-positive, it is unclear whether these findings also apply to proteinase 3 (PR3)-positive AAV patients. Further studies are required to investigate the role of mtDNA in AAV development, they said.





