ANCA-associated Vasculitis Can Sometimes Manifest as Progressive Lung Disease, Case Report Suggests
Written by |
In rare cases, ANCA-associated vasculitis (AAV) presents as an interstitial lung disease with a pattern of usual interstitial pneumonia several years before the clinical onset of vasculitis, a case report suggests.
The report, “Interstitial lung disease with usual interstitial pneumonia pattern preceding the presentation of ANCA-associated vasculitis by 4 years: coincidence or correlation?” appeared in the journal Breathe.
Interstitial lung disease (ILD) is a group of disorders characterized by impaired lung function, mostly due to lung tissue damage and scarring. While rare, some patients with pulmonary fibrosis may become positive for anti-neutrophil cytoplasmic autoantibodies (ANCAs), causing the development of AAV.
But while the occurrence of both diseases in one patient has been increasingly recognized, little is known about their relationship to each other.
In this report, Indian researchers describe the case of a 57-year-old woman who was complaining of a cough, difficulty breathing during daily activities, and weakness.
The woman had no relevant family or medical history, was not taking any medication, and did not smoke. She also did not have a history of symptoms linked to connective tissue disease or vasculitis, such as joint pains or rashes.
The patient was normal on clinical examination, other than low blood oxygen and audible fine crackles during inspiration on auscultation of the chest. Blood analysis then revealed signs of active inflammation and positivity for several autoantibodies, including anti-nuclear antibodies (ANA), rheumatoid factor, and ANCAs against the myeloperoxidase protein.
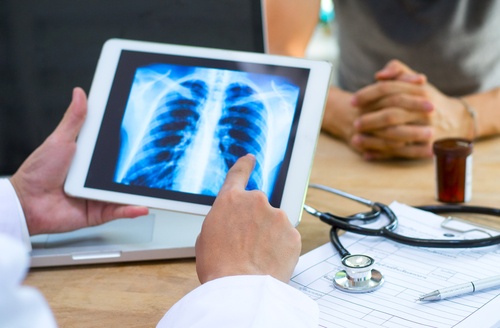
Her lung function was also compromised, exhaling significantly less air than normal and showing a reduced capacity to exchange gases. However, the team did not find any signs of pulmonary infection or vasculitis in the lung sacs, and suspected ILD with a pattern of usual interstitial pneumonia (UIP) and possible sarcoidosis.
Symptoms improved with the steroid medication prednisolone, which the patient took for one year. Three months after starting steroids, Esbriet (pirfenidone) — approved to treat idiopathic pulmonary fibrosis — and acetylcysteine were also added and continued for two years.
The patient was monitored regularly thereafter, and a routine high-resolution computed tomography (HRCT) scan conducted 3.5 years later revealed widespread lung tissue scarring.
The woman also had double vision due to nerve palsy, which resolved spontaneously, and experienced abnormal lower limb sensation with tingling, pins and needles, and cold intolerance with reduced pulse in the extremities.
A couple of months later, the patient’s little toe on the left foot was amputated due to severe tissue death and gangrene. She continued to show additional symptoms, including a rash on her lower left leg and discoloration of the second toe on her right foot.
The patient was then diagnosed with the AAV subtype microscopic polyangitis (MPA) and started taking the immunosuppressant cyclophosphamide and steroids.
“It has … been reported in a few studies that the diagnosis of ILD with UIP features often precedes the onset of features of vasculitis, particularly MPA,” the researchers wrote. “In our patient, ILD with UIP features on HRCT preceded the clinical onset of AAV (MPA) by 4 years.”
“It is important for physicians to be aware of the fact that AAV can present as an ILD with a UIP pattern,” they added. “At presentation, all patients with ILD should be assessed for AAV and tested for ANCA positivity.”
Currently, there is no specific treatment for patients with ILD and AAV, despite their worse prognosis compared with patients with only AAV. Researchers believe that further studies should evaluate if these patients could benefit of concurrent treatment with anti-fibrotic agents, “on the same lines as management of patients with UIP-ILD.”