Cocaine Use Can Trigger ANCA Production, AAV-like Kidney Symptoms, Case Reports Show
Cocaine and levamisole, a chemical substance commonly used to cut the drug, can trigger ANCA production and mimic the symptoms of ANCA-associated vasculitis (AAV), researchers said.
Most cases affect the skin and the nose, but they also can involve internal organs like the kidneys, a study including two case reports and literature review suggests. The researchers said detection of “certain clinical- and antibody constellations” should prompt drug testing, “especially in young patients,” to prevent misdiagnosis.
“Through rising cocaine consumption, cocaine and levamisole-induced AAV has become a frequently encountered form of vasculitis,” the researchers said.
The study, “Cocaine-induced ANCA-associated renal disease: a case-based review,” appeared in the journal Rheumatology International.
Regular cocaine usage can cause a condition known as cocaine-induced midline destructive lesion, which causes tissue and blood changes mimicking those of AAV. This can lead to misdiagnosis.
Cocaine is commonly adultered with levamisole, a chemical substance that also causes AAV-like symptoms. Most cases of cocaine-related vasculitis involve the skin, nose, and throat, but they can also affect internal organs like the kidneys.
Researchers in Germany and Switzerland reported two cases of cocaine-related vasculitis with kidney involvement that were misdiagnosed as AAV.
The first patient was a 19-year-old Caucasian male who had vasculitis in the skin, sinusitis, and blood, and proteins in the urine, which are markers of kidney damage. He tested positive for ANCAs.
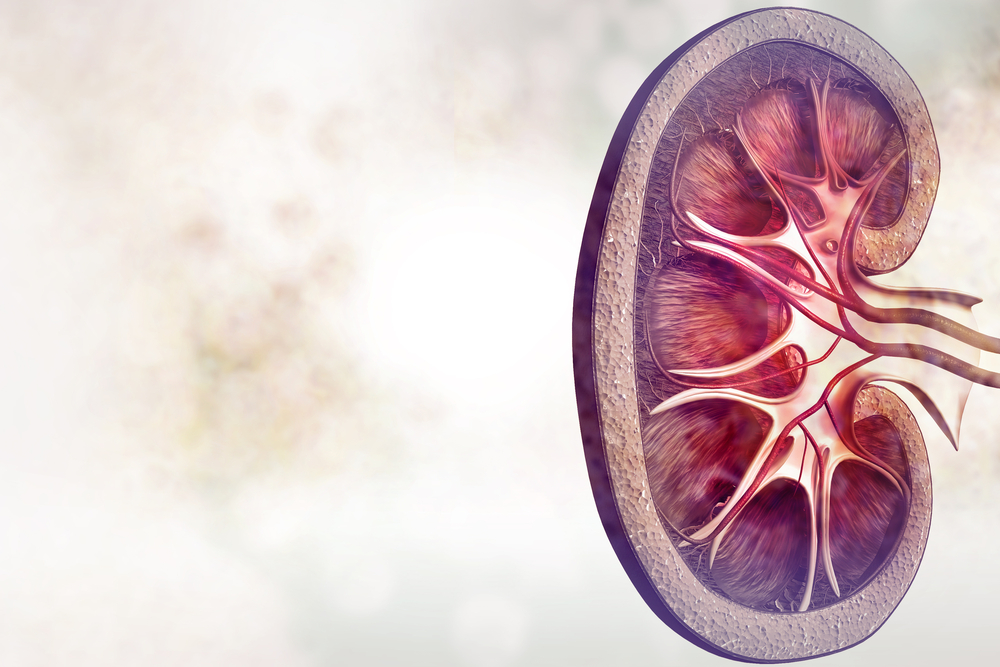
A kidney biopsy showed inflammation of the glomeruli — the filtering units of the kidney — a common manifestation of AAV.
The patient was initially diagnosed with AAV with renal involvement, and treated with prednisolone and methotrexate. However, when he reported having inhaled cocaine two weeks before the appearance of the symptoms, the doctors changed the diagnosis to cocaine-induced AAV and started treatment with Rituxan (rituximab). The patient also stopped inhaling cocaine, which was confirmed by drug tests performed during the treatment.
The symptoms in the nose, throat, and skin resolved within weeks. After six months, the patient no longer had signs of kidney damage, and was declared in full remission, the researchers said.
The second patient was a 39-year-old male who presented with nasal septum perforation — a hollow in the cartilage that separates the nostrils — sinusitis, and inflammation in the nose tissue. He also was positive for ANCAs against proteinase 3 (PR3). The man reported having inhaled cocaine occasionally in the past but denied recent usage.
The patient was diagnosed with localized ANCA-associated vasculitis and started treatment with steroids.
After four years, the patient came back to the hospital with decreased renal function and blood in the urine. A kidney biopsy showed inflammation caused by an autoimmune response. The vasculitis in his face had gotten worse, causing blindness in the right eye.
He also developed a perforation in the palate, which caused him to lose 40 kilograms (around 80 pounds) because he could not eat properly.
Drug tests screens showed cocaine consumption without levamisole. The patient refused to participate in a drug withdrawal program and was lost to follow-up.
The researchers reviewed the literature for cases of cocaine-induced vasculitis involving the kidney, and found that ANCA development is common — mostly against myeloperoxidase (MPO) or against both PR3 and MPO. Skin manifestations, anemia, and arthritis also are common.
“So far, there are no data or guidelines concerning treatment strategies in cocaine/levamisole-induced AAV with renal manifestation. Drug abstinence may be the mainstay of therapy,” the scientists said.
Most patients who stopped inhaling cocaine got better with time. However, the team noted that most patients continue to inhale the drug.
“The interpretation of the serologic markers and clinical manifestation [in cases that suggest AAV with kidney involvement] should always lead to consideration of drugs as inductors of the disease. Especially in younger patients,” the researchers concluded.
Levamisole is an anthelmintic drug — meaning “destructive to parasitic worms” — that was previously used in the treatment of tumors and other diseases characterized by immune dysfunction. However, it was pulled from the U.S. market in 2000 because of adverse effects related to its toxicity.