Scientists Identify Molecule That Triggers AAV-related Defense Mechanism
A molecule released by platelets — cell fragments in the blood that form clots and stop or prevent bleeding — appears to contribute to the progression of ANCA-associated vasculitis (AAV) by triggering a defense mechanism carried out by white blood cells.
Researchers now have identified a key signaling event present in that defense mechanism that may help identify new therapeutic targets for use against the autoimmune disorder.
Their study, “Platelet CXCL4 mediates neutrophil extracellular traps formation in ANCA-associated vasculitis,” was published in the journal Nature Scientific Reports.
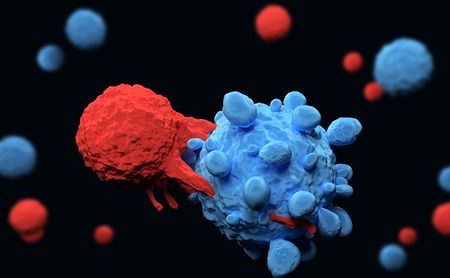
White blood cells called neutrophils participate in immune responses to infection and tissue damage by forming a “web” of extracellular DNA that traps and kills pathogens. These webs, a defense mechanism known as neutrophil extracellular traps, or NETs, are known to be involved in AAV progression.
Some studies have found evidence that platelets, a type of small cell fragment involved in clotting, can trigger NET formation, but the mechanism underlying this has not been known.
Now, scientists from the Keio University School of Medicine and the Fujita Health University School of Medicine, both in Japan, took a closer look at this relationship, investigating specific changes at the molecular level. The team compared the interactions between neutrophils derived from healthy individuals and platelets taken from both AAV patients and healthy people.
The 20 AAV patients recruited into the study had either granulomatosis with polyangiitis (GPA) or microscopic polyangiitis (MPA). They had a median age of 69, and had been diagnosed with the disease for a median of 11 months prior to the study.
The results showed that platelets from AAV patients strongly caused NET formation, while those of healthy controls or of patients with other autoimmune conditions, such as lupus and rheumatoid arthritis, did not.
A closer look at patient characteristics found that platelet-mediated NET formation was particularly high in AAV patients with lung lesions, but disease activity, levels of ANCA antibodies, or inflammation did not significantly impact this association.
The investigators next looked for changes in cell surface proteins known to interact with platelets. One such protein, called toll-like receptor 9 (TLR9), appeared much more active in AAV-associated platelets than in those from healthy controls. Between the different AAV participants, TLR9 also was more active among platelets taken from those with lung involvement than without.
“These data suggest that elevated TLR9 expression in platelets, in particular, may contribute to the principal process of pulmonary lesions in AAV,” the researchers wrote.
TLR9 is a receptor whose function — broadly speaking — is to transmit information to the platelet, usually in response to a pathogen. This triggers an inflammatory response aimed at helping the immune system clear out the invader. Following this logic, the team next examined which molecules were released by platelets when activated by TLR9.
The greatest difference occurred in the production and release of a protein called CXCL4. Blood samples of study participants supported this evidence, showing higher CXCL4 levels in AAV patients, as well as those with other autoimmune disorders, than in healthy individuals.
As a final test of CXCL4 involvement in NET formation, the investigators observed a significant increase in NET formation when healthy neutrophils were cultured with CXCL4 alone, without platelets. There also was a significant drop in NET formation after treating AAV-derived neutrophils with a CXCL4 suppressing agent.
“Taken together, our data suggest that the TLR9 − CXCL4 signaling axis is upregulated in AAV patients, promotes NETs formation and contributes to the pathogenesis of AAV,” the team concluded.
“Further evidence on the mechanisms of the crosstalk between platelets and neutrophils will aid in the identification of novel therapeutic targets for the treatment of AAV,” they added.






