Self-antibodies May Appear Years Before AAV Symptom Onset
The disease-causing autoantibodies are sometimes present long before the onset of ANCA-associated vasculitis (AAV) symptoms, with distinct disease features depending on their antibody type, a recent study finds.
Overall, the study presents “evidence of an initiation of the autoimmune process in AAV several years before appearance of the first symptoms,” the researchers wrote.
The study, “Anti-neutrophil cytoplasmic antibodies predate symptom onset of ANCA-associated vasculitis. A case-control study,” was published in the Journal of Autoimmunity.
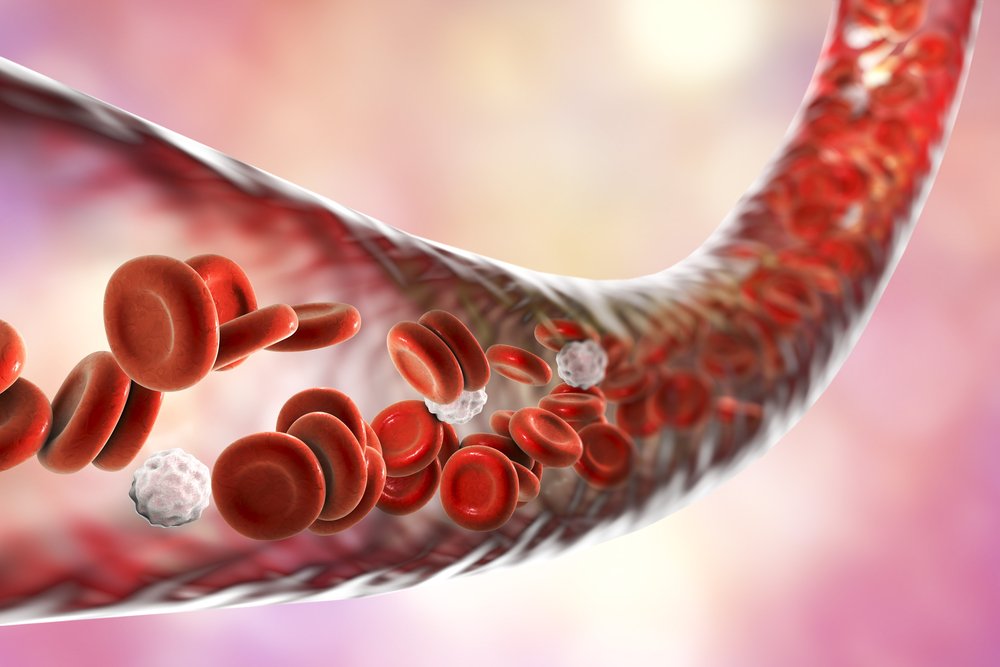
AAV comprises a group of diseases in which autoantibodies that mistakenly target the body’s own cells result in small blood vessel inflammation. These disease-causing antibodies, called anti-neutrophil cytoplasmic antibodies, or ANCAs, target proteins at the surface of certain immune cells, leading them to erroneously damage blood vessels.
In AAV, there are two major types of autoantibodies, those targeting the proteinase 3 (PR3) protein and those that target the protein myeloperoxidase (MPO).
The factors that cause antibodies against PR3 and MPO to emerge are poorly understood as is the timing of autoantibody appearance in AAV development. In the study, researchers in Sweden set out to investigate when PR3-ANCAs and MPO-ANCAs develop in relation to AAV symptom onset.
Their analysis used medical records from a Swedish patient database and included a total of 85 adults with AAV who had blood samples collected up to 10 years before their official diagnosis.
Patients with a form of blood vessel inflammation called polyarteritis nodosa were also included due to suspicion of misdiagnosed AAV. Researchers also examined samples from 170 patients, who were matched for age, sex, and blood sampling date, and served as controls.
Results showed that, even before their symptoms appeared, a greater proportion (35.7%) of AAV patients had ANCA antibodies in their blood compared with controls (3.5%). In fact, if a person showed ANCA antibodies in their blood samples, that person was 27.5 times more likely to have pre-symptomatic AAV than to be a control.
Notably, the frequency of ANCAs observed in patients increased over time until symptom onset.
Before symptom onset, 26.2% of patients developed PR3-ANCAs and 10.7% had MPO-ANCAs. Both groups were significantly associated with pre-symptomatic AAV, but PR3-ANCAs were a stronger predictor of disease.
In general, PR3-ANCAs and MPO-ANCAs appeared a median of 2.7 years and 2.0 years before symptom onset, respectively. The earliest reported PR3-ANCAs appearance was 9.7 years before symptom onset while the first MPO-ANCAs appeared 4.3 years before symptom onset.
PR3-ANCAs, however, appeared earlier in women, at a median of 6.4 years before symptoms, compared with 0.3 years earlier for men.
Additional findings continued to support that AAV manifests differently in patients with PR3-ANCAs and MPO-ANCAs. While PR3-ANCA-positive patients were younger at disease onset compared to those negative for the autoantibodies (46.7 vs. 59.3 years), patients with MPO-ANCAs were older at disease onset compared with negative patients (67 vs. 54.3 years).
Also, MPO-ANCA-positive patients more often experienced respiratory, kidney, or nervous system symptoms than patients negative for MPO-ANCAs or positive for PR3-ANCAs. In contrast, PR3-ANCA-positive patients more commonly had ear-nose-throat symptoms.
Finally, patients with PR3-ANCAs before symptom onset were more often diagnosed with granulomatosis with polyangiitis, while those with MPO-ANCAs were more often classified as having microscopic polyangiitis.
“These results add to the accumulating evidence that PR3-ANCA+ and MPO-ANCA+ AAV are distinct diseases, with substantial differences in [disease development and progression] and clinical manifestations,” the investigators wrote.
The study may be limited by its small sample size and retrospective nature, the inability to follow up with patients after disease onset, and missing or inconsistently collected patient data. Still, the researchers note that “with 85 cases included, this comprises the largest case-control study so far of the pre-symptomatic phase of AAV.”






