AAV Neutrophils Show Increased Activation of the Alternative Complement System, Study Finds
Neutrophils from patients with anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) are better at activating the alternative complement system than neutrophils from healthy people, a study has found. This research emphasizes the role of complement in AAV disease development, and suggests the therapeutic potential of its inhibition.
The study, titled “Neutrophils from ANCA-associated vasculitis patients show an increased capacity to activate the complement system via the alternative pathway after ANCA stimulation,” was published in the journal PLOS ONE.
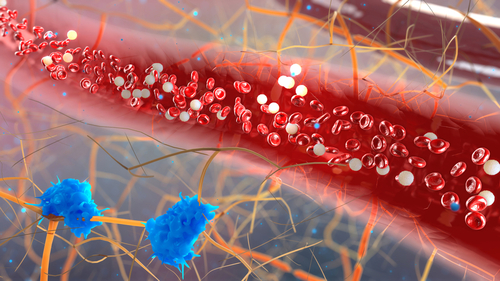
Neutrophils are immune cells sometimes called the “first responders” of the immune system — they rush to sites of inflammation, where they can help in the host defense by quickly secreting compounds that activate other parts of the immune system.
However, in AAV, the activation of neutrophils isn’t helpful as they play a well-documented role in spurring the autoimmune inflammation that’s characteristic of the disease.
Another part of the immune system that’s known to play a role in AAV is the complement system. Complement is a group of proteins that are in the blood in inactivated states, but they can quickly be activated through a domino-like series of molecular events. Once activated, the complement system can help make antibodies more potent (the system is named for its ability to “complement” antibody activity).
Although the complement system has been shown to play a role in AAV, exactly how it gets activated in AAV patients hasn’t been clear. That’s where this new study comes in.
In the study, researchers took blood samples from 10 people with AAV and 10 controls without AAV. They collected neutrophils from these samples, put the neutrophils in dishes, activated them by giving them inflammatory signals, then treated them with ANCAs (the actual autoantibodies that drive AAV) isolated from each of the 10 AAV patients.
Although neutrophils from both groups, with or without AAV, showed similar levels of overall activation, neutrophils from people with AAV produced more of a molecule called C3bBbP, which can activate the complement system through the alternative pathway. In the domino analogy, C3bBbP can “knock over the first domino.”
The data showed a great deal of variability, which is important to note. For example, while treatment with some of the ANCAs resulted in a statistically significant difference between AAV and non-AAV neutrophils, treatment with other ANCAs did not. Although the trend was generally consistent, the variability made it impossible to confidently exclude the possibility that the results were due to random chance.
The researchers then looked at possible mechanisms by which the neutrophils might be activating complement. They analyzed the neutrophils’ production of microparticles (which are basically cellular “bags” of proteins and other components used for signaling) and found that neutrophils from AAV patients made more of these microparticles than neutrophils from people without AAV.
The amount of microparticles released correlated with the amount of C3bBbP generated. When the researchers removed the microparticles, C3bBbP generation decreased significantly.
Thus, the researchers deduced that the alternative complement system in AAV is activated, at least in part, by the increased activation of neutrophils and, more specifically, by the release of microparticles from neutrophils.
“Our findings emphasize the role of complement in the pathogenesis in AAV — underlining the therapeutic potential of C5a and other complement blockade,” they concluded.






