Defense Processes of Neutrophils Linked to Active AAV Disease, Study Finds
Excessive activation of a defense mechanism of neutrophils — key immune cells in ANCA-associated vasculitis (AAV) — is a potential biomarker for active disease, according to researchers.
Their study, “Excessive neutrophil extracellular trap formation in ANCA-associated vasculitis is independent of ANCA,” was published in the journal Kidney International.
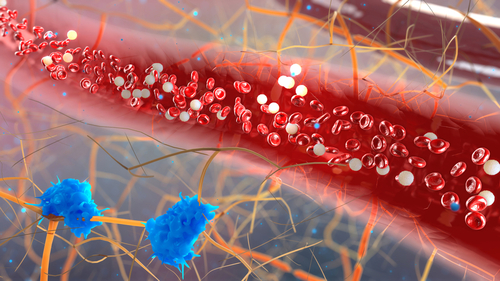
Neutrophils are a type of white blood cell involved in the inflammatory response to infection or tissue damage. One of its defense mechanisms is the formation of a type of extracellular web that traps and kills pathogens, called neutrophil extracellular traps (NETs).
Among the many antimicrobial molecules present in NETs to fight invaders are proteinase 3 (PR3) and myeloperoxidase (MPO) proteins, the most common targets of the autoantibodies produced by AAV patients.
AAV is a group of autoimmune diseases characterized by the presence of anti-neutrophil cytoplasmic autoantibodies (ANCAs) — autoantibodies against proteins present in neutrophils.
These autoantibodies wrongly activate neutrophils attached to the endothelium — the layer of cells that line the blood vessels — triggering their defense mechanisms (including NETs), which ultimately damage the walls of small vessels in different tissues and organs.
Also, activation of neutrophils’ defense mechanisms fuels the autoimmune response by exposing more PR3 and MPO in NETs to autoantibodies, and causes the production of molecules from the complement system (a major component of the immune system), which are known to amplify the activation of neutrophils.
This leads to a vicious circle, where increasing number of neutrophils are recruited and activated, amplifying the damage in AAV.
ANCA-mediated NET formation seems to be in the center of this circle, with increasing evidence suggesting that it is a key event in the development of AAV.
Researchers evaluated NET formation in 99 MPO-positive and PR3-positive AAV patients through a new highly sensitive and automated method based on laser scanning microscopy.
The method was used to quantify the formation of NETs by healthy human neutrophils exposed to blood samples of AAV patients containing the associated autoantibodies.
Blood of both types of AAV patients triggered a significant excess of NET formation compared to the blood of healthy individuals. NET formation was more highly induced by the blood of MPO-positive AAV than PR3-positive AAV patients, suggesting a potentially different role of NET formation in these types of AAV.
Also, excessive NET formation was significantly associated with blood from patients with active disease, compared with those in periods of remission or hospitalized due to severe infections.
“Excessive NET formation was associated with clinical disease activity in AAV patients and possibly distinguished autoimmunity from infection,” the researchers wrote.
These findings suggest that excessive NET formation could be used as a potential biomarker for active disease in the future, but additional larger studies are needed to clarify this potential.
To the researchers’ surprise, the levels of NET formation were not influenced by ANCA levels in the patients’ blood, nor by levels of complement molecules, suggesting that excessive NET formation was independent of these molecules.
The authors speculated that a combination of pro-inflammatory molecules and/or damage associated molecular patterns might be responsible for excessive NET formation in AAV patients.
However, since the results are clearly different than previous evidence, these possibilities must be thoroughly investigated, as well as the confirmation of the zero contribution of autoantibodies to NET formation.
The authors of a commentary published in the same issue of the journal noted that “the challenge will be to identify the exact triggers responsible for excessive NET formation in AAV patients before we can definitely conclude that the net effect of ANCA on this process is close to zero.”






