Rare Inflammatory Disorder of Brain Meninges Linked to MPO-positive AAV
A rare case of inflammatory disease affecting the protective membrane of the central nervous system was linked to anti-myeloperoxidase (MPO) autoantibodies in a case report.
The Japanese study, “A case of suspected MPO-ANCA-related hypertrophic pachymeningitis with atypical presentation,” was published in the Journal of Family and General Medicine.
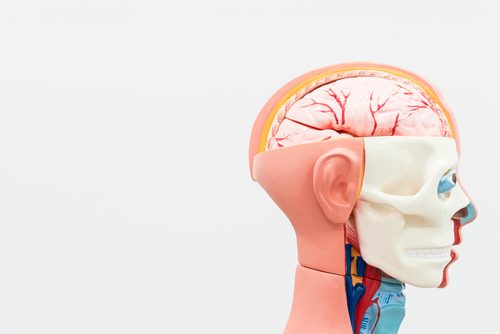
Hypertrophic pachymeningitis (HP) is a rare inflammatory disorder that leads to local or diffuse thickening of the outer membrane of the meninges, called dura mater. The meninges surround the brain and spinal cord.
The majority cases are spontaneous, with unknown causes, but secondary HP has been linked to diseases like rheumatoid arthritis, syphilis, tuberculosis, cancer, and antineutrophil cytoplasmic antibody (ANCA)-related diseases.
While some patients are completely asymptomatic, HP presents as debilitating headaches in 71.1 percent of cases, and 62.3 percent of patients have cranial nerve defects. In the latter, two or more nerves are commonly affected, and vision and hearing symptoms are frequent.
Researchers described the case of a 66-year-old man who arrived at the emergency department with impaired consciousness and headache, which had worsened over two days.
The patient had a history of chronic headaches, and had been receiving 10 mg of prednisolone for more than a year for a prior diagnosis of polymyalgia rheumatic, a joint pain disorder.
At admission, the patient was agitated, unable to follow instructions, and had a fever. While a physical exam did not reveal a specific problem, blood tests showed increased levels of white blood cells and increased C-reactive protein levels, which suggest an inflammatory condition.
Still, researchers did not find a reason for the patient’s neurological symptoms, and agreed that additional testing was needed. Enhanced brain magnetic resonance imaging (MRI) revealed thickening of the meninges (dura mater) with no additional neurological features. Based on the findings, HP was suspected.
To detect HP, “enhanced brain MRI is the most useful imaging technique,” since it can “exclude other differential diseases as required,” the researchers wrote.
The patient was started on corticosteroid treatment – 1,000 mg of intravenous methylprednisolone daily, for five days. This improved his consciousness and headaches. Lowering the dose of corticosteroids after five days did not cause his symptoms to recur.
Additional bloodwork analysis revealed elevated levels of MPO autoantibodies, supporting a final diagnosis of MPO-ANCA-related HP.
“We reported an atypical case of MPO-ANCA-related HP that presented with an acute consciousness disorder without cranial nerve deficits,” the researchers concluded.
“[Clinicians] should consider this treatable disease as a differential diagnosis when a [MPO-ANCA] patient presents with drowsiness and headache.”






